Effect of acute dose of alcohol on the biochemical features of syndrome X in different categories of male and female Nigerian drinkers in apparent good health
Innocent Onyesom, Ph.D.1, UE Uzuegbu1, G Umukoro2
1. Department of Medical Biochemistry, Faculty of Basic Medical Sciences, Delta State University, Abraka, Nigeria.
2. Department of Medical Microbiology & Parasitology, Faculty of Basic Medical Sciences, Delta State University, Abraka,
Nigeria.
Recibido para publicación julio 14, 2005 Aceptado para publicación enero 4, 2007
SUMMARY
Background: «Syndrome X», known since the 1980’s is a disease condition precipitated by insulin resistance. Insulin resistance causes glucose and insulin to accumulate in the blood. Syndrome X is characterized by abnormal values of triacylglycerol (TAG), blood pressure (BP), glucose and HDL-cholesterol-all risk factors for heart disease. Insulin resistance may be exacerbated by bad diet, poor lifestyle, absence of physical activity, genetic predisposition and being overweight. However, recent reports have shown that poor lifestyle is likely to be the main cause rather than bad diet or being overweight. Even though heavy consumption of alcohol could be regarded as a poor lifestyle, its relationship to the biochemical features and symptoms of Syndrome X in both genders is yet to be properly documented among Nigerian drinkers of alcohol.
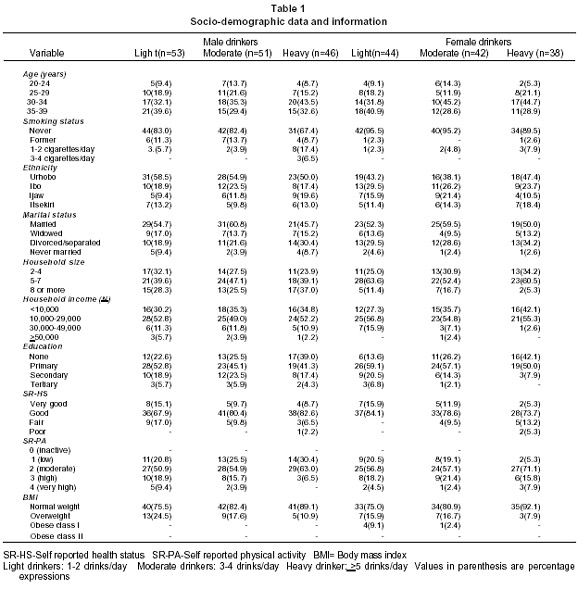
Methods: To establish a baseline information on the relationship between alcohol consumption and Syndrome X among Nigerians, two hundred and seventy-four consenting individuals in apparent good health and who were either light (53 male, 44 female), moderate (51 male, 42 female) or heavy (46 male, 38 female) drinkers of alcohol were selected. They had no personal or familial history of CHD, stroke, cancer or related diseases. The drinkers were tested using an acute dose (1 g ethanol/kg body weight) of alcohol.
Results: Results show that the administered acute dose (1 g ethanol/kg body weight) increased serum glucose, (p>0.05), TAG (p<0.05) and BP (p<0.05) some biochemical risk factors of Syndrome X in both genders irrespective of the drinking category. However, alcohol-induced changes were highest among the female heavy drinkers. Thus, observations from this study suggest that heavy consumption of alcohol by especially the female folk could alter the pathways that metabolize carbohydrates and lipids and this may increase the risk of Syndrome X.
Conclusions: Based on the available evidence, it would be reasonable to conclude that heavy consumption of alcohol by Nigerian women especially may be yet another predisposing lifestyle to Syndrome X. The incidence of Syndrome X among drinkers of alcohol should be further investigated in order to provide clues to the underlying molecular mechanisms. This is important in order to strategize therapeutic approaches, since individuals with the disease may not recognize it.
Keywords: Syndrome X; Insulin resistance; Triacylglycerol; Blood pressure; Glucose; Alcohol.
Efecto de dosis aguda de alcohol sobre las características bioquímicas del síndrome X en distintas categorías de bebedores nigerianos hombres y mujeres en aparente buen estado de salud
RESUMEN
Antecedentes: Desde la década de 1980 se conoce el síndrome X, entidad patológica que se precipita por la resistencia a la insulina. A su turno, esta resistencia hace que la glucosa y la insulina se acumulen en la sangre. El síndrome X se caracteriza por valores anormales de triacilglicerol (TAG), presión sanguínea (PS), glucosa y colesterol de alta densidad (HDL), que son todos elementos de riesgo para enfermedades cardíacas. La resistencia a la insulina se puede aumentar por malos hábitos dietéticos, falta de actividad física, predisposición genética y sobrepeso. Sin embargo, varios informes recientes demostraron que un estilo de vida poco saludable puede ser también una causa principal del síndrome, quizá más que los malos hábitos dietéticos o el sobrepeso. Aunque el consumo alto de alcohol se podría considerar como un estilo de vida poco saludable, su relación con los factores bioquímicos y los síntomas del síndrome X, en ambos géneros, aún no se ha documentado de manera precisa entre los nigerianos consumidores de alcohol.
Métodos: Establecer una información de base acerca de las relaciones entre consumo de alcohol y síndrome X para 264 nigerianos en aparente buen estado de salud que participaron de modo voluntario en el estudio. Aunque todos consumían alcohol, entre ellos había consumidores ligeros (53 hombres, 44 mujeres); consumidores moderados (51 hombres, 42 mujeres); y consumidores pesados (46 hombres, 38 mujeres). Ninguno tenía historia familiar de enfermedad cardíaca coronaria (ECC), accidentes cerebro-vasculares, cáncer, y otras enfermedades relacionadas. A todos se les examinó con una dosis de prueba (1 g de etanol/kg peso corporal) de alcohol.
Resultados: Se comprobó que la dosis de prueba administrada (1 g de etanol/kg peso corporal) aumentó los niveles sanguíneos de glucosa (p>0.05) y TAG (p<0.05), así como la PS (p<0.05), factores de riesgo para el Síndrome X en ambos géneros, sin tener en cuenta la categoría del consumidor. Sin embargo, los cambios inducidos por el alcohol fueron más altos en las mujeres de consumo pesado. Así, pues, las observaciones de este estudio sugieren que el consumo alto de alcohol, sobre todo en las mujeres, puede alterar las vías del metabolismo de carbohidratos y lípidos y de esta manera aumentar el riesgo del síndrome X.
Conclusiones: Con base en la evidencia disponible, es razonable concluir que el consumo elevado de alcohol especialmente en las mujeres nigerianas puede ser otro estilo de vida poco saludable que predispone al síndrome X. La incidencia del síndrome X entre los consumidores de alcohol se debería investigar más a fin de suministrar sugerencias e indicios acerca de los mecanismos moleculares subyacentes. Esto es importante para diseñar estrategias en los manejos terapéuticos, pues los individuos con la enfermedad no la pueden reconocer.
Palabras clave: Síndrome X; Resistencia a insulina; Triacilglicerol; Presión sanguínea; Glucosa; Alcohol.
Consumption of alcoholic beverages can influence intermediary metabolism leading to glucose intolerance1, hypertriglyceridaemia2 and hypertension3. Thus, alcohol consumption could elicit the metabolic changes observed in syndrome X, in which insulin resistance, hypertension and dislipidaemia are seen in glucose intolerant and prediabetic obese patients4. These metabolic modifications and the accompanied changes in syndrome X risk factors have been associated with a high incidence of cardiovascular disease5,6.
In Africa, particularly Nigeria, the accumulating reports on the effect of alcohol on the biochemical features of syndrome X were documented in isolation, and most of the investigations involved testing male subjects but results were usually generalized for both gender. This present study examines the effect of alcohol on the characteristic biochemical features of syndrome X in both genders using apparently healthy subjects, which include light, moderate and heavy drinkers of alcohol. It is hoped that this research report would provide clues on the potential prevalence and gender differences (if any), in syndrome X risk factors induced by alcohol ingestion.
MATERIALS AND METHODS
Subjects. Two hundred and seventy-four alcohol drinkers in apparent good health and who were either light (male=53, female=44), moderate (male=51, female=42) or heavy (male=46, female=38) drinkers were randomly selected from the major ethnic groups (Ibo, Urhobo, Ijaw, Itsekiri) in the Niger-Delta area of Nigeria after interview. From the semi-structured questionnaire, information on subjects’ social status, economic power, drinking habit and medical history were obtained. Enlisted drinkers were between the ages of 20 and 40 years, and participation was restricted to apparently healthy individuals with no personal or familial history of coronary heart disease (CHD), stroke, cancer or obvious hereditary disease. Selected subjects were then instructed to abstain from drinking alcohol two days to the scheduled period of study and only those who complied were selected and tested. The abstinence period ensures that effects observed were to a large extent, due to the acute dose (1 g ethanol/kg) investigated (administered).
Testing exercise. Upon arriving in the laboratory as scheduled, the participants willingly endorsed the form approved by our local human experimentation committee as a means of seeking their consent. They were then separated into light (1-2 drinks/day), moderate (3-4 drinks/day) and heavy (>5drinks/day) drinkers based on the semi-structured interview outcome. Their weights and heights were then taken.
The measured heights and weights were recorded to the nearest 0.1 cm and 0.1 kg, respectively. These values were used to derive the body mass index (BMI). Subjects were then divided into four BMI groups according to National Institute of Health Classification criteria7. The subjects eventually selected were tested on two consecutive days. On the first day (the control study), individuals in each drinking category were given 1 g fruit juice/kg at about 5.00 pm, after a 2 – day abstinence from alcohol. They were advised to avoid alcohol intake but allowed to eat light supper because heavy foods alter alcohol bioavailability and consequent effects. Fasting whole blood was collected the next morning at about 8.00 am after about 15 hours overnight period. On the following day (the test day), the experimental procedure was repeated as in the first day, but 1 g (30%) ethanol/kg body weight was administered in lieu of fruit juice. Pure food grade alcohol was diluted to 30% (about 60 proof) with fruit juice before being ingested. The choice of alcohol dose and interval for experimental repetition and conduct were based on previous intervention studies8,9.
Blood pressure measurements. During each occasion of testing, blood pressure was measured shortly before blood sample collection in a well-seated position after about 10 min of rest using Digital Aneroid Sphygmomanometer (ACCOSSON MERCURY, CE 0120) as previously documented8.
Blood sample collection. Blood samples were collected the next morning (around 8 am) before breakfast. Sera samples were then obtained from the collected venous whole blood by centrifuging (Vanguard V600, SmithKline Beecham) at 1200 x g for 5 min at room temperature. The separated supernatant (serum) was decanted into bijou bottle, stored frozen and analysed within 48 hours of collection.
Determination of serum glucose and triacylglycerol. Serum glucose was measured in a spectrophotometer (Photomech 301 – A: OPTIMA) by the glucose oxidase method10 using a Randox kit, Ardmore, United Kingdom. Serum triacylglycerol was determined by a spectrophotometer (Photomech 301 – A: OPTIMA) using the end-point colorimetric method11 and reagent kit supplied by Teco Diagnostics, USA. The spectrophotometric assays at Vantex Research and Diagnostic Laboratory met the standards of the Centers for Disease Control and Prevention Lipid Standardization Program.
Risk factor categories. Blood pressure was classified according to current guidelines12. Triacylglycerol levels were classified according to the National Cholesterol Education Program guidelines13, and based on fasting glucose levels, subjects were classified as having normal glucose, impaired fasting glucose or diabetes in accordance with the American Diabetes Association guideline14.
Statistical analysis. Analysis of variance (ANOVA) was used to compare group mean values, followed by the Newman-Keuls post-hoc test15 to determine statistical significance between the groups. Differences were considered significant when p<0.05.
RESULTS
The socio-demographic data (Table 1) shows that heavy drinking of alcohol may affect physical activity, marital status and household size/income. Evidence (Table 1) suggests that illiteracy may influence the pattern of alcohol consumption. Illiterates are more likely to drink more, especially among the Urhobos and Ijaws. Majority of the participants had normal weight as judged by the BMI values. There were no marked gender differences in the socio-demographic statistics so presented.
The experimental data obtained (Table 2) show that the control values of serum glucose, triacylglycerol and blood pressure for the heavy drinkers were highest when compared with those of the light and moderate drinkers, and the degree of differences were more among the females. Similar trend was observed during the test experiment. These present results indicate that alcohol consumption increases blood glucose, blood triacylglycerol and blood pressure–the symptoms (or risk factors) of syndrome X, in both genders but more in female heavy drinkers.
DISCUSSION
The term, «syndrome X» was introduced during the early 1980’s, and since then, the disease is just beginning to attract serious concern. It has been estimated that about one third of the adult population in the developed world have syndrome X, and they do not know it. Syndrome X is the term used for a cluster of conditions that tend to appear in some individuals, and symptoms include glucose intolerance, hyperlipidaemia and hypertension, and it is common among prediabetic, obese individuals. The disease condition is also known as metabolic syndrome and many researchers think that it is genetically based, but poor lifestyle is likely to be the main cause. Subsequent research findings have shown that even if one looks after oneself, eat a low-fat diet and are not obese, one could still be at a considerable risk.
The biochemical features of syndrome X alter pathways involving the metabolism of both carbohydrates and lipids4, and these alterations may lead to glucose intolerance (probably arising from insulin insensitivity), dyslipidaemia, and hypertension. The data obtained from this investigation show that alcohol consumption increases serum glucose, triacylglycerol and blood pressure Table 2), and these present observations agree with earlier isolated reports on the effect of alcohol on blood glucose1,16, serum triacylglycerol2, and blood pressure3,8. Thus, apart from the positive relationship between central obesity and syndrome X, heavy consumption of alcohol by women especially, appears to be a potential predisposing lifestyle, this study suggests.
The metabolic relationship between syndrome X risk factors and alcohol consumption is beginning to emerge2. Alcohol-induced increase in NADH/NAD+ ratio raises the concentration of glycerol-3-phosphate and this leads to high plasma glucose as a result of decreased peripheral utilization of glucose17. This condition may elicit insulin release, and consequently, insulin resistance (syndrome X) could develop when too much insulin circulates in the blood for too long, because the body’s cells have to protect themselves from being overcome by too much glucose.
Increase in glycerol-3-phosphate also favours triacylglycerol synthesis and its hepatic accumulation18, and alcohol-induced increase in serum triacylglycerol has been reported19. Increases in blood triacylglycerol concentrations have been shown to reduce the number of insulin receptors20. There is also a growing body of evidence linking plasma triacylglycerol to the «clogging» of arteries, which may increase the risk of heart attack or stroke. High triacylglycerol alone increases the risk of heart attack nearly three-fold, and people with the highest ratio of triacylglycerol to HDL -the «good» cholesterol- had 16 times the risk of heart attack as those with the lowest ratio21. Some researchers now think that plasma triacylglycerol levels may actually be more important than cholesterol levels in establishing heart disease risk.
We conclude that heavy consumption of alcohol may be yet another cause of the metabolic adaptations that could promote fat formation. This could culminate in hypertriglyceridaemia, a condition known to induce poor glucose tolerance, oversecretions of insulin and higher risk of heart disease. However, restricted carbohydrate diet has been reported to be beneficial in reducing the level of blood triacylglycerol in compliant patients21. The guidelines for this dietary intervention should be fully developed for possible therapeutic application, especially now that changing customs appear to condole (women) drinking of alcohol even publicly, and coupled with the fact that syndrome X can hardly be recognized by sufferers. Thus, such dietary approach to the treatment of syndrome X should be properly investigated, because it could be bestowed with the prowess of averting the progress of the subtle disease in alcoholics, when possibly coupled with the advise to reduce or avoid alcohol consumption.
ACKNOWLEDGEMENTS
The authors wish to appreciate the cooperation of the subjects, and the management of Vantex Research and Diagnostic Laboratory, Sapele, Delta State, Nigeria.
REFERENCES
1. Badawy A. A-B. A review of the effect of alcohol on carbohydrate metabolism. Br J Alcohol Alcoholism 1977; 12: 120-136.
2. Hodge AM, Dowse, GK, Collins VR, Zimmet PZ. Abnormal glucose tolerance and alcohol consumption in three population at high risk of non-insulin dependent diabetes mellitus. Am J Epidemiol 1993; 137: 178-189.
3. Rakic V, Puddey IB, Burke VD, Dimmitt SB, Beilin LJ. Influence of pattern of alcohol intake on blood pressure in regular drinkers: a controlled trial. Hypertension 1998: 16: 165-174.
4. Reaven GM. Banting lecture 1988: Role of insulin-resistance in human disease. Diabetes 1988; 37: 1595-1607.
5. Defronzo RA, Ferranini E. Insulin-resistance. A multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 1991; 14: 173-194.
6. Reaven GM, Laws A. Insulin-resistance, compensatory hyperinsulinaemia and coronary heart disease. Diabetologia 1994; 37: 948-952.
7. National Institute of Health National Heart Lung and Blood Institute. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: the evidence report. Obes Res 1998; 6 (Suppl): 51-210.
8. Moreira LB, Fuchs FD, Moraes RS, Bredemeier M, Duncan BB. Alcohol intake and blood pressure: the importance of time elapsed since last drink. J Hypertens 1998; 16: 175-180.
9. Onyesom I. Changes in blood pressure and plasma urate induced by the metabolism of alcohol in humans. Global J Med Sci 2003; 2: 157-160.
10. Trinder P. Quantitative determination of glucose using GOD-PAP method. Ann Clin Biochem 1969; 6: 24-27.
11. Searcy RL. Diagnostic biochemistry. New York: McGraw Hill; 1961.
12. Chobanian AV, Bakris GL, Black HR, et al. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood pressure: the JNC 7 Report. JAMA 2003; 289: 2560-2571.
13. National Cholesterol Education Programme (NCEP) Executive Summary of the Third Report of the Expert Panel on Detection, Evaluation and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001; 285: 2486-2497.
14. American Diabetes Association. Diagnosis and Classification of Diabetes mellitus. Diabetes Care 2004; 27 (Suppl): 5-10.
15. Winer BJ, Brown DR Michels M. Design and analysis of single-factor experiment: completely randomized design. In: Statistical Principles in Experimental Design. New York: McGraw Hill Inc; 1991. p. 74-418.
16. Lieber CS. Medical and nutritional complications of alcoholism: Mechanisms and management. New York: Plenum Press; 1992.
17. Sereny G, Endrenyi L, Devenyi P. Glucose intolerance in alcoholism. J Stud Alcohol 1975; 36: 359-364.
18. Onyesom I, Obodoruku S, Imafidon EE. The influence of duration of alcoholism on plasma triacylglycerol, lipoprotein cholesterol and blood pressure in Nigerian alcoholics. J Med Lab Sci 2000; 9: 93-98.
19. Onyesom I, Osioma E. Dose-dependent changes in plasma triacylglycerol and blood pressure induced by alcohol in humans. Nig J Biochem Mol Biol 2001; 16 (Suppl): 139-141.
20. Bieger WP, Michel G, Barwich D, Bienhl K, Wirth A. Diminished insulin receptors of monocytes and erythrocytes in hypertriglyceridemia. Metabolism 1984; 33: 982-987.
21. Mercola J. Triglycerides may predict heart risk. Circulation 1997; 96: 2520-2525.