Impact of Moderating Model of the Risk in the Chronic Renal Disease. IPS COMFANDI, Cali, 2006
Luis Mariano Otero, M.D.1,2, Alvaro Muñoz, M.D.1,3, Lunevar Figueroa, M.D.1
1. Physician, Caja de Compensación Familiar (COMFANDI), Quality Assurance Department, Subdirección de Salud, Cali, Colombia. e-mail: lunevar@yahoo.com
2. Coordinator of Postgraduate Nephrology Program, Internal Medicine Department, Universidad del Valle, Cali, Colombia.
3. Epidemiologist, Colombian Foundation for Brain Trauma Management (FUNDCOMA), Cali. Colombia. e-mail: alvaro.munozc@telecom.com.co
Recibido para publicación enero 19, 2006 Aceptado para publicación julio 4, 2007
SUMMARY
Objective: To assess if a health care model implemented at the basic level of the IPS COMFANDI and based on an early intervention in cardiovascular risk factors and its application to patients with different levels of chronic renal disease, produces significant changes in lab and clinical parameters to be translated into stabilization or regression of the disease.
Materials and methods: From the cardiovascular risk program 362 patients were randomly selected with different stages of renal disease, diabetes mellitus (DM), and arterial hypertension, (AHT). Two measurements were made: one before and another after the intervention, with an interval of six months. Wilcoxon hypotheses were tested to compare means of clinical interest and lab variables as well as dynamics of change in the number of patients according to KDOQUI stage, for both periods.
Results: A total of 8 factors were evaluated: 4 clinical and 4 lab parameters, as well as patients’ proportion according to nephropathy stage (KADOQUI) found in the two periods. Clinical variables were measured for 24 hours such as systolic, diastolic and mean blood pressure and proteinuria which showed differences before and after the intervention that were statistically significant. BMI (body mass index), glycemia and microalbuminuria did not present statistically significant differences for the two measurements.
Conclusion: Implementation of a basic level health care model focused on risk reduction for renal chronic disease, by means of an intensive therapy, has also an affirmative incidence on diseases such as diabetes and hypertension. Results are favorable when measuring key variables in renal chronic disease and suggest a positive impact regarding this important public health problem in Colombia.
Keywords: Primary prevention; Natural history of the disease; Testing hypothesis; Regression; Stabilization; Epidemiological transition.
In Colombia a transition process is taking place regarding population growth and epidemiology with lower fertility rates and higher life expectancy. However, the disease load is characteristic of developing countries such as acute diarreic disease, maternal mortality, etc., higher morbility and disabilities due to chronic diseases and their consequences (1).
Chronic renal disease incidence in LatinAmerica and Colombia has had an unprecedented growth similar to levels found in industrialized societies. At present, in the city of Cali and Valle Department (State), more than one thousand patients are receiving dyalisis, accounting for almost 15% of all patients in Colombia. The Hospital Universitario del Valle has doubled the cases of terminal renal failure during 2001 and 2002 when compared to 1999 and 2000 (2).
Health care institutions face a challenge because the health prevention approach has to continue as well as the definition of effective strategies that respond to the integral management of chronic entities such as hypertension and diabetes, diseases specific to elderly people that tradi-tionally have been a matter of concern only to developed countries.
Since health care to these patients implies a high cost that the health care system finds difficult to be compensated, researchers have gone beyond the understanding of the natural history of the disease looking for alternatives that may have a timely impact with a cost-effective approach.
This is the reason to adopt a model that emphasizes intervention on cardiovascular risk (3) factors in order to have an early incidence on chronic renal disease.
Among other aspects, this model has a practical approach regarding:
· Specific therapy based on diagnosis
· Evaluation and management of morbid conditions going with
· Delay in renal function loss
· Cardiovascular disease prevention and treatment
· Renal function reduction prevention and treatment of complications
An intensive therapy characterized by a strict control of glucose in diabetic people and blood pressure in hypertensive patients in order to improve glomerular rate filtration (GRF) or creatinine clearance (4).
This therapy is implemented by nephrologists strategically located in primary health care centers who have trained general physicians and with almost exclusive medication from the obligatory health plan (OHP), have been able to enhance solutions by integrating inclusion and patient follow-up processes from a biopsicosocial perspective.
According to the epidemiological profile (Muñoz A., October 2006 unpublished data) at COMFANDI from a total of 230,000 members affiliated, 10% have a diagnosis of chronic arterial blood hypertension and 2% diabetes mellitus, and an intermediate group of 6% to 7% of patients with different levels of renal function reduction (nephropathy).
The definition of renal chronic disease (not renal failure) in accordance with K/DOQUI (4-6) (kidney disease outcomes quality initiative) is:
1. Renal failure for more than three months, considered as structural or functional kidney abnormalities with or without GFR (glomerular filtration rate) decrease.
2. GFR below 60 ml/min, 1.73 m2 for a period over three months with or without evidence of kidney dammage.
In this case, GFR was considered as the output variable (GFR normal value 60 to 120 ml/min/1.73).
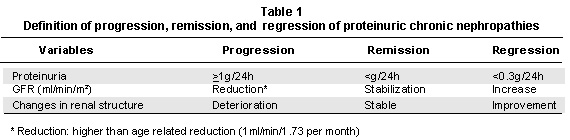
The working hypothesis assumes that the so called risk moderating model is able to produce a favorable impact in renal chronic disease. This is demonstrated by propitious changes in clinical and lab parameters between the two measurements (before and after) y is translated into Remission or Regression of this pathology (Table 1) (6-9).
MATERIALS AND METHODS
Retrospective data were collected from clinical histories of patients attending regularly the cardiovascular risk program in nine (9) primary IPSs from COMFANDI between 2005 and 2006.
Inclusion criteria were male and female patients having a certain stage of chronic renal disease with two GFR measurements, one at time zero and the second one at least six months after starting the intervention.
Following KDOQUI recommendations to estimate GFR in patients with a renal chronic disease, the prediction equation based on creatinine or the «Cockcroft-Gault equation» (5-6) was used, because it gave a more accurate measurement and includes variables such as age, sex and additionally incorporating 100% of observations.
KDOQUI establishes that the loss of physiological GFR associated to aging is 1 ml/min/1.73 per year and it defines an accelerated deterioration of renal function as a loss of 4 ml or more per minute per year.
As it was decided to assess stabilization and/or regression in a six month period, 2 ml were considered as the minimal difference to be found between the measurements. Independent variables were 8 in total: 4 clinical and 4 lab (Table 2).
Dependent variable was creatinine clearance or GFR, expressed as 1 to 5 gradients that increase their value according to severity in renal function loss, where 1 represents the lowest value and 5 an indication for dyalisis:
Stage 1 = GFR normal or above 90 ml/min/1.73m2
Stage 2 = GFR 60 to 89
Stage 3 = GFR 30 to 59
Stage 4 = GFR 15 to 29
Stage 5 = GFR <15
Statistical analysis. In 2005 from 13,216 patients included in the cardiovascular risk program with a diagnosis of hypertension and/or diabetes, in around 6 % (792) a certain degree of kidney chronic disease (6-16) was found.
Since it was expected to find small differences such as a GFR of 2 ml from the first to the second measurement, with an 89% power, a 95% significance and a 0.9 correlation ratio, 360 patients had to be taken in.
As a compensation for losses sample size was increased by 10%, and 396 patients were selected through a simple random sampling; among them 34 were excluded because they lacked one of the two measurements and 362 were included in the final analysis.
The study design was a «before and after» analysis with «no control group», each subject was his own control. Wilcoxon allocated range test was used, considering the large sample size (n>15) and the fact that the addition of ranges is normally distributed and as a result z statistical analysis (18,19) was utilized.
First, an univariate analysis of population characteristics such as age, weight and independent variables was carried out including a comparison of means, medians and standard deviation with a gender control. Later, age and weight performance were analyzed according to gender and IPS.
Then, correlation charts were drawn for systolic, diastolic and mean blood pressures and for GFRs for both periods and including gender stratification.
Wilcoxon allocated range tests were carried out for each of the clinical and lab variables in the two periods.
Finally, to determine the rate of patients migrating within their category from time zero and postintervention, GFR variable was grouped in 5 categories (kadoqui) and was likened by means of a ratio comparison test with chi2.
STATA 8.0 statistical package was applied through all of the statistical analysis.
RESULTS
Tables 3 and 4 present the summary for clinical and lab variables. From a total of 362 individuals, 214 (60%) were males and 148 (40%) females, with a mean age of 64 years for both groups. In average, males were 12 cm taller than females.
For both groups, median age was 63 years. However, at the Candelaria IPS the mean age was 48 and the median 49 years, the youngest group. Average weight for all the population was 71 kg during both measurements but it was higher in males (74 kg) when compared to females (66 kg).
Clinical parameters. In relation to BMI, a mean of 27.5% and a median of 26.89 was obtained for the first period and a value of 27.72 for the second one. These differences are statistically significant (p=0.03) although the patients remained within the same overweight category (BMI = 25% to 29%).
Median systolic blood pressure (SBP) presented a significant reduction of 8 mm Hg from to the first to the second measuremnt (p=0.000).
Although in diastolic blood pressure (DBP) the median was similar for both measurements when age stratification was used, it was found that only in the 15 to 44 group or only in 36 subjects of the population under study, there were no differences (p=0.8), while in groups from 45 to 64, 65 to 74 and 75 and over, differences were significant from the first measurement to the second one (p=0.000).
Mean blood pressure (MBP) was reduced by 5 mm Hg in the median between the first and second measurements, and represented a 5% significance (p=0.000).
In both periods, the rate of reduction of SBP was higher when compared to DBP and MBP (Table 5).
Laboratory parameters. For creatinine, even if data had a small reduction from time 1 (1.37 mg%) to time 2 (1.26 mg%), this reduction was enough to show statistically significant differences (p=0.000).
After the intervention, mean and median values were lower for microalbuminuria but overall there was not an important reduction (p=0.15). This finding did not change when gender and age groups stratification were implemented.
Microalbuminuria presented the lowest number of paired data (39) with a wide range, data scattering and a variation ratio of 137%.
For fasting blood sugar, the median for time 1 was 120 mg% and postintervention reached 119 mg%, a 1 mg% reduction not producing a statistically significant change (p=0.24),but when a gender stratification was made a reduction in females but not in males was found. In the case of males, the mean and the median figures did not vary from time 1 to time 2.
In relation to proteinuria at 24 hours, a significant reduction was present (p=0.000) from 251 mg to 171 during time 2, although a large data scattering were present with a variation ratio of 171%, a posible explanation for the large range variation and the lower number of observations (184).
In the result variable, GFR increased from time 1 to time 2 with a median before the intervention of 52 ml/min/m2 and after of 55 ml/min/m2, which was significant (p=0.000). Gender stratification showed statistically significant differences from time 1 to time 2 (female p=0.000) (male p=0.000). Chart 1, shows similar results in relation to statistical significance that were obtained when stratifying per age group. Larger differences were found for the median in the group from 15 to 44 years (Chart 2).
K/DOQUI stage. Category 3 presented the highest prevalence, 49% for basal time and 42% after the intervention. The intervention allowed migration of 24 patients in category 3 in time 1 to time 2, 18 showed a regression, 15 to stage 2 and 3 to stage 1, the remaining 6 presented a progression, 4 to stage 4 and 2 to stage 5. When implementing ratio comparison tests, it was found that in the evolution of patients in time according to the category, there was a marginal statistical significance p=0.06 in category 3 of kdoqui classification; in other categories differences were not significant (Table 6).
DISCUSSION
At present, in Colombia there are no similar publications assessing the impact of an intervention in patients with chronic kidney disease. This is the main strength of the study.
The design did not include a control group for moral reasons: it was not ethical to deprive patients from the benefits of a therapy assessed as effective in other countries, since biological responses are similar in all of the human beings.
In public health, some interventions need to produce rapid responses vis-à-vis a changing reality, therefore programs must be implemented and/or evaluation designs that can not always comply with all recommendations from «lex art» in epidemiology. Besides, given the type of intervention and the non-inclusion of a control group in the design before and after the use of subjects as their own control, the only option available was to control external factors that may be a threat to the conclusions validity.
It is important that neither weight nor BMI showed a reduction in the postintervention measurement although the benefits of weight reduction to control blood pressure and blood sugar levels in patients with cardiovascular disease and/or metabolic syndrome were widely proved.
On the other hand, it is worth increasing the efforts to capture patients in early stages of cardiovascular disease even before the onset of renal function deterioration. As it is shown on Chart 2, the group from 15 to 44 years had the highest response in terms of a larger delta change in GFR increase by 12 ml/min/m2.
In terms of K/DOQUI category classification, in this study it was observed the highest prevalence of patients in category 3 which was the only one showing an important reduction in the number of patients from time 1 to 2.
Microalbuminuria was the co-variable with a lower number of observations (39), as per protocol in COMFANDI, this test is given only at month seventh after the patient is officially included in the cardiovascular risk program.
As a large number of patients had a diagnosis of diabetes, it would be desirable in a future study to have values for glycosilated hemoglobin as an additional marker of patient evolution (6-9).
Once a positive impact may be established for this intervention, the next step would be to consider factors related to this success.
There are several studies indicating a correlation between chronic kidney disease and cardiovascular disease (6-16), in future cohorts it could be appropriate to examine the relation between intervention and incidence rates for cardiovascular disease.
CONCLUSION
Results in favor of an alternate hypothesis suggest that it is likely that differences found could be due to intervention and not to other foreign factors. In similar studies with a larger period between the two measurements, it is expected to find relevant differences in all the variables of interest.
Multiple conditions imposed by the public health reality in Colombia, force to implement novelty health care models that involve the best scientific evidence and are susceptible of evaluation in terms of impact.
ACKNOWLEDGMENTS
This study has received logistic support from different areas of COMFANDI health care management from areas such as service networks, health promotion and statistics. Authors would like to express their gratitude to physicians, nurses and in general to field workers for their valuable contribution in data management.
REFERENCES
1. Organización Panamericana de la Salud. La salud en las Américas. Volumen II. Washington: Oficina Sanitaria Panamericana; 1998.
2. Otero LM. Enfermedad renal crónica. Colomb Med 2002; 33: 38-40.
3. Servicio Occidenhttp://www.bmj.com/cgi/reprint/333/7571/733tal de Salud. Modelo de atención moderador de riesgo. Cali: Servicio Occidental de Salud, Publicaciones; 2006.
4. NKF-K/DOQI. Clinical practice guidelines for chronic kidney disease. Am J Kidney Dis 2002; 39 (Suppl 1): 76-79.
5. Traynor J, Mactier R, Geddes C, Fox J. How to measure renal function in clinical practice. BMJ 2006; 333: 733-737.
6. Rule AD, Gussak HM, Pond GR, Bergstralh EJ, Stegall M, Cosio FG, et al. Measured and estimated GFR in healthy potential kidney donors. Am J Kidney Dis 2004;43: 112-119.
7. Locatelli F, Manzoni C, Marcelli D. Factors affecting progression of renal insufficiency. Miner Electrolyte Metab 1997; 23: 301-305.
8. Klausen K, Borch-Johnsen K, Feldt-Rasmussen B, Jensen G, Clausen P, Scharling H, et al. Very low levels of microalbuminuria are associated with increased risk of coronary heart disease and death independently of renal function, hypertension and diabetes. Circulation 2004; 110: 32-35.
9. Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis 1998; 32 (Suppl 3): 112-119.
10. Shulman NB, Ford CE, Hall WD, Blaufox M, Simon D, Langford HG, et al. Prognostic value of serum creatinine and effect of treatment of hypertension on renal function. Results from the hypertension detection and follow-up program. The hypertension detection and follow-up program cooperative group. Hypertension 1989; 13 (5 Suppl): 180-193.
11. Shlipak MG, Heidenreich PA, Noguchi H, Chertow GM, Browner WS, McClellan MB. Association of renal insufficiency with treatment and outcomes after myocardial infarction in elderly patients. Ann Intern Med 2002; 137: 555-562.
12. Hakim RM, Lazarus JM. Progression of chronic renal failure. Am J Kidney Dis 1989; 14: 396-401.
13. Culleton BF, Larson MG, Parfrey PS, Kannel WB, Levy D. Proteinuria as a risk factor for cardiovascular disease and mortality in older people: a prospective study. Am J Med 2000; 109: 1-8.
14. Iseki K, Ikemiya Y, Fukiyama K. Risk factors of end-stage renal disease and serum creatinine in a community-based mass screening. Kidney Int 1997; 51: 850-854.
15. Wachtell K, Ibsen H, Olsen MH, Borch-Johnsen K, Lindholm LH, Morgensen CE, et al. Albuminuria and cardiovascular risk in hypertensive patients with left ventricular hypertrophy: the LIFE study. Ann Intern Med 2003; 139: 901-906.
16. Hillege HL, Fidler V, Diercks GF, van Gilst WH, De Zeeuw D, van Veldhuisen DJ, et al. Urinary albumin excretion predicts cardiovascular and noncardiovascular mortality in general population. Circulation 2002; 106: 1777-1782.
17. Anavekar NS, Gans DJ, Berl T, Rohde RD, Cooper W, Bhaumik A, et al. Predictors of cardiovascular events in patients with type 2 diabetic nephropathy and hypertension: a case for albuminuria. Kidney Int Suppl 2004; 92: 50-55.
18. Shewskin D. Handbook of parametric and nonparametric statistical procedures. 2nd ed. Boca Raton: Chapman & Hall/CRC; 2000.
19. Siegel S, Castellan N. Estadística no paramétrica aplicada a las ciencias de la conducta. 4ª ed. México: Trillas; 1995.
20. Gordis L. Epidemiología. 3ª ed. Baltimore: Elsevier; 2005.