Coexistence of psoriasis and vitiligo
María Isabel Moreno, MD1, Luis Hernando Moreno, MD2
1. Resident, Dermatology Service, Department of Internal Medicine, School of Medicine, Faculty of Health, Universidad del Valle, Cali, Colombia. e-mail: mimoreno@imbanaco.com.co
2. Auxiliar Professor, Department of Internal Medicine, School of Medicine, Faculty of Health, Universidad del Valle, Cali, Colombia. e-mail: luis.moreno@imbanaco.com.co
Received for publication September 26th, 2007 Accepted for publication September 18th, 2008
SUMMARY
We present a 53-years old male with a 10 years history of vitiligo who further developed psoriatic lesions clearly representing a Koebner´s phenomenon. He is currently being treated with phototherapy and narrowband UVB with an interin satisfactory outcome especially in the psoriasis.
Keywords: Psoriasis; Vitiligo; Koebner´s phenomenon.
Coexistencia de psoriasis y vitiligo
RESUMEN
Se presenta el caso de un paciente de 53 años de edad, con historia de 10 años de evolución de vitiligo y quien posteriormente, sobre estas lesiones, desarrollo psoriasis en placas, manifestándose como un fenómeno isomórfico de Koebner. En la actual recibe tratamiento con fototerapia, luz ultravioleta B de banda estrecha, con resultados satisfactorios especialmente en la psoriasis.
Palabras clave: Psoriasis; Vitiligo; Fenómeno de Koebner.
CLINICAL CASE
A 53 year-old male patient, with diabetes which is under control with metformina and glibenclamida, presented macules with absence of pigment compatible with vitiligo 10 years ego. He developed lesions on his upper limbs, elbows, back of hands. Subsequently he presented the same lesion in the anterior region of his knees; after two years scaly erythematosus greyish-bronze colour with metallic sheen papules and plaques were observed over those injuries, which is not expressed in healthy skin. He received topical treatments several times without any improvement in an outlying medical health centre.
At the physical examination acronym macules were found localized in the flexor region of the elbow, back of hands, anterior region of knees and malleolus.
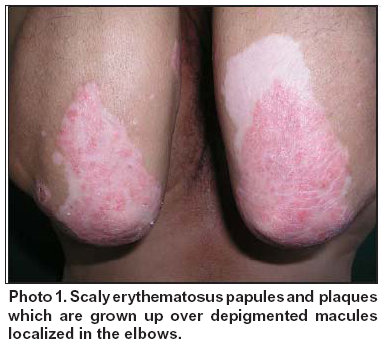
Those lesions were observed under the fluorescente light of Wood and clinical correspondences with vitiligo lesion; on each of the lesions grew up scaly erythematosus greyish-bronze colour with metallic sheen papules and plaques regular and well-defined edge, which respect to healthy skin compatible with plaque psoriasis (Photo 1).
At the histopathological study was found epidermal hyperplasia, parakeratosis, with deep papillaes cori, few lymphocytic infiltratesmall and decrease in the number of melanocytes, which was confirmed by fontana coloration; reporting presumptive diagnostic of psoriasis (Photo 2).
It was decided to start handling with light narrow-band ultraviolet B, there was an improvement in the psoriasis lesions approximately 70%; however the depigmented macules were still present. Currently the patient is under treatment (Photo 3).
DISCUSSION
The vitiligo is a skin diseases aetiology has yet to be recognized. It is manifested clinically as acronyms macules or depigmented circumscribed generally well-defined edges. It has been found that the functional melanocytes disappear from the affected skin. There are several hypotheses on the pathogenesis of this disease, especially theory of immune kind by the presence of antibodies directed against of melanocytes antigens. Recent researches have given importance to the antibodies and directly cellular cytotoxic aimed against the melanocytes, is unusual to find cases associated between vitiligo and autoimmune diseases behaviours such as diabetes and thyroiditis.
Psoriasis is a chronic disease usually asymptomatic, it is characterized by well-defined edges, erythematosus greyish-bronze colour with metallic sheen plaques. There are several sort clinical forms of it like psoriasis vulgaris, which is characterized by the presence of localized lesions usually on the elbows, knees, sacral region, scalp and nails. Gutatte psoriasis is a clinical type which appears small spots, it is associated with infection by Streptococcus. Also there are several forms of this entity as psoriatic arthritis, erythrodermic and pustular psoriatic.
Histologically psoriasis presents epidermal hyperplasia, proliferation of keratinocytes and acanthosis, papillomatosis, parakeratosis and lymphocytic infiltrate usually low. Its aetiology is unknown and presents an auto-immune behaviour. So far it is believed that its pathogenesis is multifactor, immune disorders type has been important where T cell plays an important role, like the neurogenic changes, showing an increase in the concentration of neuropeptides1,2.
Although the association between psoriasis and vitiligo were described since 1890, the relationship between these two diseases is not clear. It has been suggested that the decline or absence of melanin might be a predisposing factor for developing scalyerythematous plaques of psoriasis; its impact on dark-skinned people is low compared with patients in pale skin.
There are different types of auto-immune mechanisms which can lead to this correlation. It has been found that both diseases share as HLA haplotypes as t CW * 6 and B * 27; the common neuropeptides, which increased the levels of tumor necrosis factor alpha, it induces neurotoxins from melanocytes in vitiligo patient. Also that increased has been found in patients with psoriasis.
Both diseases have a high production of pro-inflammatory molecules such as interleukin-1, interleukin-6, interleukin-8, tumor necrosis factor, nuclear factor-kB and peptide vasoactivo2-4.
Another cause that can produce coexistence between psoriasis and vitiligo is the Koebner isomorphic phenomenon response which is characterized by the appearance of lesions on healthy skin, which has been subjected to a traumatic process that would stimulate fibroblast growth factor released by keratinocytes injured leading to a proliferation of endothelial cells. This phenomenon was found in psoriasis and vitiligo, in both individually and in other skin diseases such as lichen planus. In addition it described a similar reaction in some viral entities such as verruca vulgaris and diseases of betaman, although in those cases is attributed to contagion.
Therapies for the management of these two diseases, both topical and systemic and combined, are similar in the vast majority of patients. Phototherapy is an especially good choice for narrowband UVB, being a first-line treatment of the diseases described in this case, with satisfactory results4,5.
In conclusion, we present the case of a patient who developed papules and plaques of psoriasis lesions on vitiligo as a phenomenon of Koebner isomorphic. These two entities shared pathogenesis and clinical behaviour auto-immune and neuropeptides that make them immunologically similar. His topical and systemic therapy in many cases is similar.
REFERENCES
1. Berger TG, Klesewetter F. Psoriasis confines strictly to vitiligo areas- a Koebner like phenomenon? J Eur Acad Dermatol Venereol. 2006; 20: 178-83.
2. Sandhu K, Inderjeet K. Psoriasis and vitiligo. J Am Acad Dermatol. 2004; 51: 149-50.
3. De Sica AB, Wekelin S. Psoriasis vulgaris confined to vitiligo patches and occurring contemporaneously in the same patient. Clin Exp Dermatol. 2004; 29: 434-5.
4. Ujiie H, Sawamura D. Development of lichen planus and psoriasis on lesions of vitiligo vulgaris. Clin Exp Dermatol. 2006; 31: 375-7.
5. Weiss G, Shemer A. The Koebner phenomenon: review of the literature. J Eur Acad Dermatol Venereol. 2002; 16: 241-8.