Thrombosis in renal artery in a newborn. Presentation a review of a case
Ana Lucía Torres, MD1, Javier Torres, MD2, Jorge Andrés Cifuentes, MD3
1. Neonatology Resident, Departamento de Pediatría, Escuela de Medicina, Facultad de Salud, Universidad del Valle, Cali, Colombia.
2. Assistant Professor, Departamento de Pediatría, Escuela de Medicina, Facultad de Salud, Universidad del Valle, Cali, Colombia.
3. Assistant Professor, Departamento de Radiología, Escuela de Medicina, Facultad de Salud, Universidad del Valle, Cali, Colombia.
Received for publication Novembre 26, 2007 Accepted for publication January 15th, 2009
SUMMARY
This report describes a newborn who presents high pressure values and absence of pulses in inferior extremities in his 4th day of life. Posterior to placement of umbilical arterial catheter, confirming diagnostic of thrombosis in aorta and left renal artery. A gamagraphy with MAG 3 was performed that gave evidence of left renal exclusion and aorta and left renal angioresonance. A management with no fractional heparin and streptokinase during 6 hours was initiated. The compromise in lower extremities was totally recovered, improving presure values in a few days. Following studies of renal function and growth give evidence of left renal artery flow and some function. This report describes an improvement with anticoagulant and thrombolitic treatment of a newborn kidney depite of a prolonged ischemia.
Keywords: Aorta thrombosis; Renal thrombosis; Newborn hypertension; Renal isquemia; Anticoagulan; Thrombolitic.
Trombosis de la arteria renal en un recién nacido. Presentación de un caso y revisión
RESUMEN
Se describe un neonato que presenta cifras tensionales elevadas y ausencia de pulsos en miembros inferiores en su cuarto día de vida después de la colocación de un catéter umbilical arterial, evidenciando trombosis en arteria aorta y renal izquierda. Se realizó gammagrafía con MAG 3 que mostró exclusión renal izquierda y angioresonancia de aorta y renal izquierda. Se inició manejo con heparina no fraccionada y estreptoquinasa durante 6 horas. Se recuperó totalmente el compromiso en miembros inferiores, mejorando cifras tensionales a los pocos días. Estudios de seguimiento de función renal y crecimiento evidencian flujo de arteria renal izquierda y algo de función. Se describe mejoría con tratamiento anticoagulante y trombolítico de un riñón neonatal a pesar de sufrir isquemia prolongada.
Palabras claves: Trombosis aorta; Trombosis renal; Hipertensión neonatal; Isquemia renal; Anticoagulante; Trombolítico.
This pathology has been recognized over the last decade due to the use of umbilical arterial and venous catheterization. Vascular spasms occur as a result of arterial constriction and in early stages may be difficult to distinguish them from thrombolytic states, which generally are followed by pallor and cyanosis of the limbs after the insertion of catheters1,2. This complication may result in damages to different organs, migration of thrombus, embolization to other areas and infections. At artery level, compromise may extend to the aorta and its ramifications to lower limbs, renal and cerebral. Systemic therapy with fibrinolytic agents continues to be controversial. However, treatment with these agents is considered to be positive in spite of their use several days after the diagnostic took place.
REPORT OF THE CASE
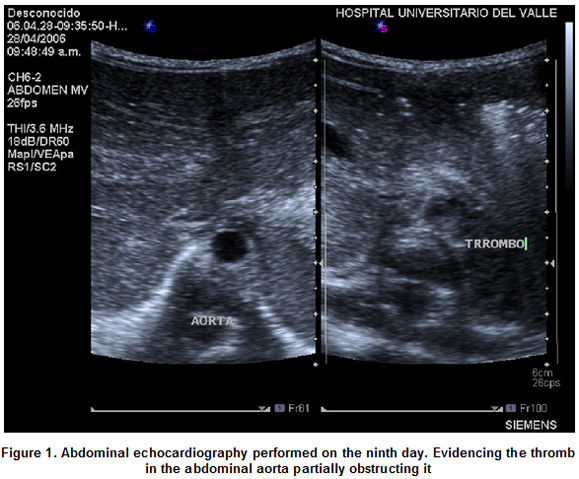
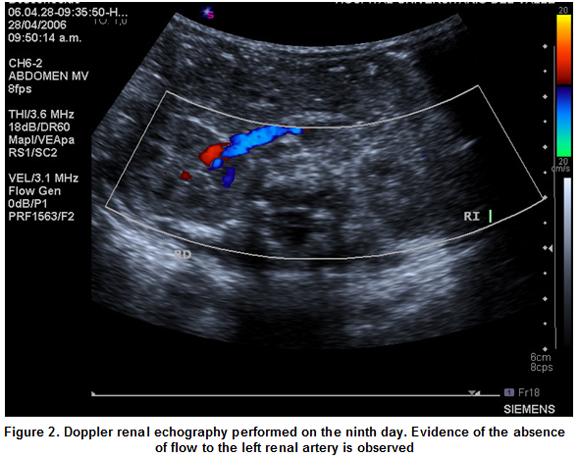
The case was present at the Neonatal Unit (CIRENA) of the Hospital Universitario del Valle. Corresponds to a masculine neonatal of 34 weeks, weighing 2,035 g, hospitalized for presenting signs of breathing difficulties, for which the umbilical venous and arterial catheterization was performed. On his fourth day of life, the patient presents high blood pressure and on the seventh day acrocyanosis is evidenced, absence of pulsations and arterial tension in the lower limbs is not present. on the eighth day the umbilical catheters are removed, the patient continues to be hyper tense and changes in his lower limbs, previously described are present. Echocardiography is performed observing a thromb at the aorta level. The diagnostic was confirmed on the ninth day by means of a doppler echocardiography (Figures 1, 2) which evidenced a thromb partially compromising the aorta and completely compromising the left renal artery by not detecting blood flow to the left kidney.
The anticoagulants protocol was initiated with non fractioned heparin (initial Dose 75 U/k/hour and continued with 20 U/k/hour) and endovenous thrombolytic therapy y with endovenous estreptokynase (4,000 U/k/initial dose and continued with 2000 U/k/hour for six hours). High blood tension persisted until the sixteenth day in spite of medical antihypertensive treatment and that the perfusion and flows to the lower limbs was completely recovered eight days after having initiated the thrombolytic handling of the patient. The patient was evaluated by a medical board which requested a renal gammagraphy with MAG 3 (Figure 3) and an abdominal and renal angioresonance (Figure 4a, b, c), which evidenced the absence of the left renal function and absence of blood flow to the left lower limb and left kidney respectively.
Antihypertensive treatment was continued (propanolol) and with oral anticoagulants (warfarin). At the age of three months a doppler renal echography control was performed which evidenced growth of the left kidney and with a DMSA Renal Gamagraphy which evidenced function of the left kidney. Arterial tension, creatinine, growth and development of the left limb were normal during the following six months. A doppler renal echography control was performed evidencing asymmetry in renal dimensions (right kidney length: 4.9 cm; left kidney 3.5 cm) evidencing flow in the left renal parenchyma (Figure 5a, b).
DISCUSSION
The frequency of vascular complications associated with the use of arterial umbilical catheters in neonates is relatively high. Approximately 30%, depending of the diag-nostic method and the symptomatology of the patient´1-5.
Clinical signs such as the absence of pulses, changes in color of the limbs, hypertension, hematuria and oliguria confirm the diagnostic. Verification may be made through angiographies but in some instances may prove to be of difficult access. Doppler Echography is also available but sensitivity and specificity may be uncertain1,2. A detailed clinical history of ancestor and family members presenting thrombolyc and thrombolitic processes must be recorded.
The first step for the management of the process is to provide support care that must include paraclinic studies such as electrolytes, correction of anemia, sepsis, thrombocytopenia and the removal of catheters. The therapy with anticoagulants consist mainly of the use of standard or not fractioned heparin (HNF), low molecular weight heparins (HBPM) and thrombolytic therapy, with or without surgical intervention. Surgical intervention will be assessed accordingly with the degree of severity of the thrombus1-3.
Arterial hypertension due to reno vascular lesion is common in survivors of neonates presenting aortic lesions. A study, with a four year follow up performed by Seibert et al.6 documented renal growth impairment in 78% of the survivors of aortic thrombolysis. Many authors conclude that the absence of renal blood flow may early predict an irreversible renal lesion having high mortality rates. We initiated treatment in spite of the diagnostic made several days after the occurrence of the event, with previous valuations and strict follow up with fibrinogen, dimer D, coagulation times and hemograms. This case suggests a recovery of the perfusion in the left inferior limb and in the renal function, in spite of the appearance of a ischemia interval of nine days; accepting the theory that an immature kidney may tolerate better a hypoxic ischemia without a time limit for defining the treatment.
The management of this pathology in the neonatal stage is controverted and is performed based on cases reported and studies extrapolating the reports of descriptive studies on children. The therapy for neonates must be considered in an individual manner and the risk-benefit of each treatment must be assessed together with the possible compromise of vital organs1-4.
Finally a strict follow up must take place during the infancy period evaluating the presence of hypertension, renal function anomalies and growth and development of lower limbs.
REFERENCES
1. Ramasethu, Jayashree. Management of vascular thrombosis and spasm in the newborn. NeoReviews. 2005; 6: c298- c310.
2. Thornburg C, Pipe S. Neonatal thromboembolic emergencies. Semin Fetal Neonatal Med. 2006; 11: 198-206.
3. Seventh ACCP Conference on Antithrombotic and Thrombolytic Therapy. Chest. 2004; 126 (Suppl): 645-87.
4. Michaels L, Gurian M, Hegyi T, Drachtman R. Low molecular weight in the treatment of venous and arterial thromboses in the premature infant. Pediatrics. 2004; 114: 703-7.
5. Coleman M, Spear M, Finkelstein M, Leef K, Pearlman S, Chien C, et al. Short-term use of umbilical artery catheters may not be associated with increased risk for thrombosis. Pediatrics. 2004; 113: 770-4.
6. Seibert J, Northington F, Miers J, Taylor B. Aortic thrombosis after umbilical artery catheterization in neonates: prevalence of complications on long-term follow-up. AJR. 1991; 156: 567-9.