Kangaroo mother program: physical growth and morbidity in a cohort of children, followed from 40 weeks of postconceptional age until first year
Diana Palencia, Enf1, Carlos Julio Mendoza, MD2, Javier Torres, MD3, Carlos Armando Echandía, MD4
1. Nurse Coordinator, Kangaroo mother program, Hospital Universitario del Valle, Cali, Colombia.
e-mail: esterpa12@hotmail.com
2. Resident, Department of Pediatrics, School of Medicine, Faculty of Health, Universidad del Valle, Cali, Colombia.
e-mail: cmendoza6@unab.edu.co
3. Assistant Professor, Department of Pediatrics, School of Medicine, Faculty of Health, Universidad del Valle, Cali, Colombia. e-mail: torres@andinet.com
4. Assistant Professor, Department of Pediatrics, School of Medicine, Faculty of Health, Universidad del Valle, Cali, Colombia. e-mail: cechandia@emcali.net.co
Received for publication February 22, 2008 Accepted for publication July 1, 2009
SUMMARY
Introduction: Up to 40 weeks of postconceptional age, the kangaroo mother program at the Hospital Universitario del Valle has proved to be a safe alternative for premature babies’ management with a low birth weight.
Objectives: To evaluate the physical growth and morbidity in children followed since 40 weeks up to 1 year in the program.
Material and methods: A cohort study was performed in newborn infants admitted to the kangaroo mother program in the newborn unit at the Hospital Universitario del Valle, Cali, Colombia, with birth weight lower than 2000 g, from 40 weeks postconceptional age up to one year age, between August 2002 and July 2006. Information was collected about maternal age and morbidity, prenatal control, type of birth, gender, birth weight, gestational age, breastfeeding, thick motor development, physical growth, morbidity, readmissions, mortality and tests results.
Results: A total of 390 infants were admitted to the program, with a 61% of captation. 65% of theirs mothers did not have prenatal control. Before completing the 40 weeks, 5.3% were readmitted due to anaemia and apnoea. After 40 weeks, 13% were readmitted by bronchopneumonia and acute diarrhoea. Most of them were allocated in the reference percentiles for weight and size. Size had a better growth than weight. The cumulated low weight incidence for age at 13 months was 22%.
Conclusions: To increase the coverage of prenatal control program and to watch that the children receive prescribed iron and formulated folic acid.
Keywords: Kangaroo mother; Low birth weight; Under nutrition; Follow-up; Cohort.
Programa Madre Canguro: Crecimiento pondoestatural y morbilidad de una cohorte de niños seguidos desde las 40 semanas de edad postconcepcional hasta los 12 meses
RESUMEN
Introducción: Hasta las 40 semanas de edad postconcepcional, el programa madre canguro del Hospital Universitario del Valle, ha mostrado ser una alternativa segura para el manejo del prematuro con bajo peso al nacer.
Objetivos: Evaluar el crecimiento pondoestatural y la morbilidad en los niños seguidos desde las 40 semanas de edad postconcepcional hasta el año en el programa.
Materiales y métodos: Se evaluó la cohorte de niños que ingresaron al programa madre canguro en la unidad de recién nacidos del Hospital Universitario del Valle, Cali, Colombia, con peso <2,000 g, desde las 40 semanas de edad post-concepcional hasta el año de edad, entre agosto de 2002 y julio de 2006. Se recogieron datos sobre edad y morbilidad materna, control prenatal, vía de nacimiento, género, peso al nacer, edad gestacional, lactancia materna, desarrollo motor grueso, crecimiento físico, morbilidad, reingresos, mortalidad y resultado de pruebas.
Resultados: Ingresaron 390 lactantes al programa con una captación de 61%. En 65% de sus madres no hubo control prenatal. Antes de completar las 40 semanas, 5.3% se hospitalizaron por anemia y apneas; después de las 40 semanas, 13% por bronconeumonía y diarrea aguda. La gran mayoría se ubicó dentro de los percentiles de referencia para peso y talla. La talla tuvo un mejor crecimiento que el peso. La incidencia acumulada de peso bajo para la edad a los 13 meses fue 22%.
Conclusiones: Aumentar la cobertura del programa de control prenatal y vigilar que los niños reciban el hierro y el ácido fólico formulados.
Palabras clave: Madre Canguro; Bajo peso al nacer; Desnutrición; Seguimiento; Cohorte.
In 1988 the Hospital Universitario del Valle (HUV) starts following infants discharged from intensive care and medial neonatal care, residing in Cali. After 1992 this follow up was performed only in premature newborn babies, minor 1500 g, based in medical literature referring them as higher risk neonatal complications and residual problems during first year of life1,2.
Due to an overcrowding of 170% in these areas during 2001, and a program follow up captation of only 30% of discharged patients, nurse Diana Palencia was send to training to the «Casita Madre Canguro» of San Ignacio Hospital and the intensive care neonatal unit at the Social Security in Bogotá3,4. And from August, 2002, the Program Madre Canguro (PMC) was started in the Newborn Unit at the HUV, as a strategy to increase survival of premature newborns, and to reduce occupational and hospital infection rate4,5.
In July 31, 2003 first evaluation point for this follow up5, the PMC showed to be a safe alternative to management low birth-weight children. 66 out of 80 babies in the program, reached 40 weeks of age, 93% receiving maternal lactation, with an average weight gain of 15 g/kg/day; only 3 children (4.5%) were readmitted, with no mortality. This study was done in order to further assess the children of low birth weight followed in the PMC, specifically their weight-growth and morbidity, once fulfilled 40 weeks of post conceptional age up to 1 year in the program.
MATERIAL AND METHODS
A cohort study was continued with admitted children to the PMC from newborn nursery at the HUV, from August 2002 to July 2006, followed from 40 postconceptional week age up to one year old, with the following inclusion criteria to begin an intrahospital program:
1. Newborn babies <2000 g birth weight.
2. Thermoregulation and respiratory pattern appropriate with normal oxygen saturation.
3. From the city of Cali and that do not plan to be out of town.
4. Mother and/or family willing to collaborate with the follow-up program accepting indications and attending controls
Inclusion criteria for discharge to home:
1. Infants with adequate heat regulation.
2. That can suck, suckle and breathe coordinately.
3. Adequate weight gain.
Exclusion criteria:
1. Be referred to another institution.
2. To have large or lethal malformations
3. Early serious conditions as hypoxic-ischemic encephalopathy, pulmonary hypertension, grade III/IV intraventricular haemorrhage
KANGAROO MOTHER PROTOCOL PROGRAM
Hospital intervention. As soon as neonates co-ordinately may suck, breast-feed and breathe, have a thermal regulation, daily weight gain and with a willing family, they may be accepted in the program. Within the neonatal unit, mother heat is used as a loving incubator to the low-weight neonate, maintaining the kangaroo position (skin contact between mother and baby, in a vertical position in the middle of the mother´s breast and under her close), permanent breastfeeding, oxygen saturation and daily weight control, with a goal to increase between 15 and 20 g/kg/day. If weight gaining is not satisfactory, maternized milk is added with a dropper or a spoon. If after one week, weight gain is adequate, maternized milk will be progressively reduced.
Ambulatory intervention. Regardless weight or post-conceptional age, and after an adequate training, the newborn is discharged with kangaroo position 24 hours/day until rejected. Receiving permanent breast-feeding and daily visits monitorizing adequate weight gain. When this is accomplished, will be started weekly visits until 40 weeks age and then at 1st, 4th, 7th , 10th and 13th month of corrected age. Ambulatory kangaroo equipment is formed by a multidisciplinary team of paediatricians, psychologists from admission, ophthalmology after 32 weeks and physical therapy, phonoaudiology, pediatric odontology and occupational therapy from 40 weeks.
Measurements. Information was collected about maternal age and morbidity, prenatal control, birth way, gender, gestational age, birth weight, APGAR score, mother lactation, gross motor development through the INFANIB test and physical growth measured as weight in grams, size and cephalic perimeter in centimeters at birth, at discharge, at 40 weeks of gestational age, at 1st, 4th, 7th, 10th and 13th age month. These last variables were compared to US Health Statistics National Center (NCHS)6. Morbidity, readmissions, mortality and audiometric test evaluation, auditory evoked potentials and transfontanellar ultrasound.
Collecting and processing information. All of this information was collected during follow-up consultations, in a created format for the study and then digitized in a Data Base create on the Epi-info 2004 statistical package for analysis. Each studied variable was edited, seeking for lacking data or errors for immediate correction and to describe them in absolute and relative frequencies the categorical and by means of averages, ranges and standard deviation of the continuous variables.
Ethical aspects. According to administrative, scientific and technical norms for health investigation, Resolution No. 08430, 1993 from former Health Ministry, present study has a minor than minimal risk, because it is a periodic information recollection, during a lactating cohort follow-up program. It was evaluated and approved by the Ethics Committee of the Hospital Universitario del Valle and the Human Ethics Committee of the Faculty of Health of the Universidad del Valle.
RESULTS
During the period comprised between August 1, 2002 and July 31, 2006, were presented in the HUV 2328 live born babies, less than 2000 g, which 557 died (24%); were excluded from program 832 (35.7%) by being referred to other institutions, 85 (3.6%) for serious congenital malformations, 66 (2,8%) with severe hypoxic ischemic encephalopathy, 111 (4.7%) due to pulmonary hypertension and 38 (1.6%) for intraventricular haemorrhage (IVH) grade III to IV. From 639 children candidates for PMC participation, 390 were admitted with a 61% of captation.
The mother’s average age was 24 years (7 year standard deviation), 65% did not have prenatal control and most frequent diagnosis were blood hypertension and pre-eclampsia (41%), urinary infection (15%), vaginosis (15%) and early rupture of ovular membrane (10%). 58% were born by Caesarean section, mainly due to pre-eclampsia, with the next averages (range in parenthesis) 31 weeks (25-38), gestational age (SD 2.3) and 1,413 g (550-1,999) birth weight (SD 310 g). Male gender had a bigger birth weight than female, 1,473 g than females 1,353 g (p= 0.007). No difference in size was found.
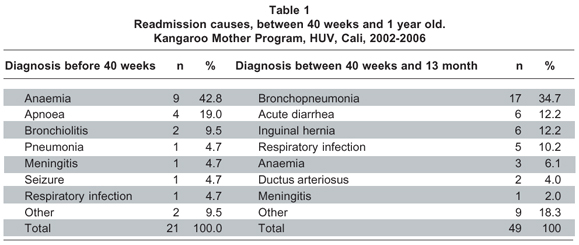
Before completing 40 week post conceptional age, 3 neonates deserted and 21 (5.3%) were readmitted, mainly with anaemia, apnoea and bronchiolitis, with no mortality (Table 1).
The cohort assembled at 40 weeks of postconceptional age, had 387 infants, 51% breast-feeding, and 43% complemented with formula milk. Average weight 2,789 g (1,420-4,680 range). No differences were found in average weight or size for gender. 89 (23%) had low weight for age and 41 (10.5%) had a low weight for size (<3 percentile, CNHS)6. From 150 children with transfontanellar ultrasound, 12 (8%) had abnormal reports, half of them with IVH. From 176 acoustic emissions 19 (10.7%) children showed hypoaccusia, and from 92 auditory evoked potentials, 9 (9.7%) children confirmed hypoaccusia, for a hypoaccusia prevalence of 2.3% in the cohort.
Between 40 weeks of postconceptional age and 13 months age, 15 children deserted, 34 were out the program for change of city and 49 (13%) were readmitted, mainly for bronchopneumonia, acute diarrheal disease, inguinal hernia and high respiratory infection with no deaths (Table 1).
In July 31, 2006, cut point in the study, 198 (51%) children had 13 months age and 140 (36%) had not reached that period. From the first group 115 (58%) were girls and 83 (42%) were boys. With an average weight of 8,987 g (6,780 to 12,320 g range), male gender had a larger weight/size average than females (9,270/8,704 g (p=0.0001) and 75.6 cm vs. 74.6 cm (p=0.031). After this follow up to 13 months, the accumulated incidence of low weight for age was 22% (44 children) and low weight for size was 12.6% (25 children), below third reference percentile CNHS6.
Referent to weight and size growth of these 198 children, the weight for age in girls was between the reference values of CNHS up to 4th month life, at that period, low weight girls increased below 3rd percentile until about 50% at 13 months (Graphic 1). The weight for age in boys remained about 25% below percentile 3 up to 7th month and increased up to half at 13 months (Graphic 2).
Half of the 89 children with low weight for age at 40 weeks age, recovered weight, entered in the CNHS percentiles and ended at 13 months age with an adequate weight for age. Other 50% ended follow up with low weight for age.
76% of 41 children with low weight for size, at 40 weeks age recovered weight, entered in the CNHS percentiles and ended at 13 months age with adequate size for age. Other 24% ended with a low weight for size.
Half of 44 children with low weight for age, at 13 month age, had started follow up with an adequate weight, but lowered percentiles to end below 3rd.
80% of 25 children with low weight for size, at 13 months age, had started follow up with an adequate weight, but lowered percentiles to end below 3rd.
Length for girls’ age was in CNHS percentiles during the 13 months follow up. Graphic 3. Length for age in boys during the first months was within the percentiles, but ended at 13 months 25% below the 3rd percentile (Graphic 4).
During follow-up consults the most frequent observed morbidity in this group was common cold (29%), acute diarrheal disease (11%), bronchiolitis (10%) and bronchial reactivity (9%). Respect to mortality, a telephone contact with children families was done and there was no mortality up to study cut.
DISCUSSION
PMC at the newborn nursery in HUV, maintains a high captation of eligible newborn babies <2000 g birth weight (61%) giving early discharge to an important number lowering stay and possibly accumulation, crossed infections and morbi-mortality7,8. Also increasing skin-to-skin contact with their mothers, breast-feeding (94% with feeding up to 40 week), with all known benefits from maternal milk, psychological, immunologically and nutritionally9,10, the empowerment and compromise from these mothers with their children and decreasing the rate of child abuse and neglect.
Only 35% of mothers from this children group assisted to prenatal control and the diseases observed during pregnancy (pre-eclampsia, urinary infections and vaginosis) are part of the risk factors reported in the world literature associated to prematurity and low birth weight11,12. An increase in the coverage of prenatal care program for pregnant women would make a very cost-effective prevention of these entities and would decline the presentation of prematurity and low birth weight11,12.
5.3% of these children were readmitted before 40 weeks mainly with anaemia and secondary apnoea, with necessary red cell transfusion in the emergency department. Besides, these children do not accumulate enough iron and other elements reserves due to prematurity, and do not get the iron and folic acid prescribed on discharge. Being ferropenic anaemia a highly prevalent and silent entity in Colombian media, rarely diagnosed and corrected, and with many repercussions for the capacity of attention, learning, muscle work, cell immunity and susceptibility to infections in children who have it13.
13% were readmitted at 40 weeks and 13 months age mainly with respiratory infection, bronchopneumonia and acute diarrheal disease, coinciding with the 2 most frequent consult causes in clinical practice in Cali media14.
A 2.3% confirmed hypoaccusia by auditive potentials in this lactating cohort, similar figure found in neonatal sift of hypoaccusia in health neonates from Hall et al.15 where they indicate this as a universal test due to the great impact in language development and cognisance that implies a diagnostic delayed.
It should be noted what was observed in the growth charts for weight and height during 13 months of follow-up, in this group of children born with weight of 1,413 g and average length of 41 cm; at 40 weeks of postconceptional age and in the following months, the vast majority were located within the reference percentiles CNHS.
The growth in height for age, during this follow-up was longer within the percentiles of reference than the weight growth for age. Size values in girls were normal during the 13 months, the boys completed with a 25% lower percentile 3 for age. Referring to growth of the weight for age, 50% of children ended up with low weight for age.
Cumulated incidence of low weight for age was 22%-23% at 40 weeks and 13 months. Cumulated incidence of low weight for size was 10.5% at 40 weeks and 12.6% at 13 months, low-considered data that can be considered low given the weeks of gestation, weight and size at birth and all the hardships and entities suffered in the neonatal stage.
CONCLUSIONS
1. PMC at newborn unit from HUV maintains a high captation of eligible <2,000 g (61%) babies, early discharging an important number, reducing piling up, cross infections and morbimortality. Increasing skin-to-skin contact with mothers, breast-feeding, empowering and compromising these mothers with their children and reducing infant abuse and neglect.
2. Increasing covertures of prenatal control program to pregnant women might do a very cost effective prevention of entities such as preeclampsia, urinary infection and vaginosis and reducing prematurity and low birth weight11,12.
3. Premature babies with low birth weight are not receiving iron and folic acid supplementation, readmitting 5.3% before 40 weeks, mainly for anaemia and secondary apnoea due to anaemia.
4. It should be noted what was observed in the growth charts for weight and height during 13 months of follow-up, in this group of children born with weight of 1,413 g and average length of 41 cm; at 40 weeks of postconceptional age and in the following months, the vast majority were located within the reference percentiles CNHS.
5. The growth in height for age, during this follow-up was longer within the percentiles of reference than the weight growth for age. Size values in girls were normal during the 13 months.
Interest conflict. The authors declare that there are no interest conflicts in this manuscript.
RECOMMENDATIONS
1. Covertures should be increased in the prenatal control program up to 100% pregnant women, to control diseases such as eclampsia, urinary infection and vaginosis, and reduction of low birth weight neonates and premature.
2. Watch and follow up discharged lactants for iron and folic acid supplementation, to reduce anaemia frequency and its repercussions on learning, activity and infection control.
3. Apply confirmatory sift tests such as otoacustic emissions, auditory evoked potentials, ophthalmology tests, INFANIB test and psychomotor developing scales to detect and early treat auditive, visual and neural development alterations.
REFERENCES
1. Escobar GJ, Littenberg B, Petitti D. Outcome among surviving very low birth weight infants: A meta-analysis. Arch Dis Child. 1991; 66: 204-11.
2. Blackman JA. Neonatal Intensive care: Is it worth it? Developmental squealed of very low birth weight. Pediatr Clin North Am. 1991; 38: 1497-508.
3. Martínez H, Rey E, Navarrete L, Marquette C. Programa Madre Canguro en el Instituto Materno Infantil de Bogotá. Primer Encuentro Internacional del Programa Madre Canguro. Bogotá: UNICEF; 1990. p. 21-43.
4. Currea S. El método canguro para el manejo del niño prematuro. En: Rojas E, Sarmiento F. (ed.) Pediatría. Diagnóstico y tratamiento. 2ª ed. Bogotá: Celsus; 2003. p. 186-95.
5. Torres J, Palencia D, Sánchez DM, García J, Rey H, Echandía C. Programa Madre Canguro: primeros resultados de una cohorte de niños seguidos desde la unidad neonatal hasta las 40 semanas de edad postconcepcional. Colomb Med. 2006; 37: 96-101.
6. Hamill PVV, Drizd TA, Johnson CL, Reed RR, Roche AF. NCHS growth curves for children from birth to 18 years. United States. Publ. N° (PHS) 78-1650. Vital Health Stat. 1977; 11: 1-74.
7. Polin RA, Saiman L. Infecciones intrahospitalarias en la unidad de cuidados intensivos neonatales. Pediatr Rev. 2003; 24: 363-70.
8. Charpak N, Ruiz JG, Charpak Y. Programa Madre Canguro Rey-Martínez: ¿una vía alternativa para el cuidado de los recién nacidos de bajo peso? Mortalidad al año en un estudio de dos cohortes. Pediatrics. 1994; 38: 338-44.
9. Lemons P, Stuart M, Lemons JA. Breast feeding the premature infant. Clin Perinatol. 1986; 13: 111-22.
10. Steichen JJ, Krug-Wispe SK, Tsang RC. Breast feeding the low birth weight preterm infant. Clin Perinatol. 1987; 14: 131-71.
11. Ortiz E. Estrategias para la prevención del bajo peso al nacer en una población de alto riesgo, según la medicina basada en la evidencia. Colomb Med. 2001; 32: 159-62.
12. Bergonzoli G, Núñez H. Futuro de la desnutrición intrauterina en neonatos a término. Colomb Med. 1997; 28: 182-7.
13. Sarmiento F. Anemia nutricional del niño. En: Rojas E, Sarmiento F. (ed.) Pediatría. Diagnóstico y tratamiento. 2ª ed. Bogotá: Celsus; 2003. p. 883-9.
14. Palau JM. Tratamiento antibiótico en infección respiratoria alta. Curso continuo de actualización en pediatría. PRECOP. 2003; 4: 33-54.
15. Hall JW, Smith SD, Popelka GR. Newborn hearing screening with combined otoacustic emissions and brainstem auditory evoked. J Am Acad Audiol. 2004; 15: 414-25.