Acute retinal necrosis
Hugo Hernán Ocampo, MD1, Alexánder Maximiliano Martínez, MD2
1. Cirujano de Retina y Vítreo, Clínica de Oftalmología de Cali, Colombia. e-mail: hhocampo@gmail.com
2. Residente, cuarto año de Oftalmología, Sección de Oftalmología, Departamento de Cirugía, Escuela de Medicina, Facultad de Salud, Universidad del Valle, Cali, Colombia. e-mail: alexmart75@gmail.com
Received for publication October 5, 2007 Accepted for publication July 1, 2009
SUMMARY
Purpose: Clinical features in a case of acute retinal necrosis are described as well as its diagnostic approach and response to early treatment.
Methods: This is a descriptive and retrospective study case report of a 26 year old male patient who arrived to the emergency room with a three day history of sudden visual loss in the right eye (RE). At initial evaluation a visual acuity of hand movements in the RE, 20/15 in the left eye (LE) and a right relative afferent pupillary defect were found. Fundoscopy revealed profuse soft exudates and hemorrhages involving posterior pole, inferior hemiretina and superotemporal periphery. Infectious workup and fluoresceinic angiography were made and positive serologies for herpes virus types 1 and 2, without HIV, were found. A diagnosis of acute retinal necrosis was made and treatment with intravenous valgancyclovir for two weeks and intra-vitreous triamcinolone for severe vasculitis, was given. Then a 3 months treatment with oral antiviral agents was prescribed.
Results: Patient’s evolution showed improvement with treatment and at two and a half months of follow up, visual acuity was 20/50 in the right eye, normal slit lamp examination, tonometry of 12 mm Hg and fundoscopy improved when compared to initial pictures.
Conclusions: A high index of suspicion is needed for diagnosing ARN taking into account clinical findings. Prompt intravenous and intra-vitreous treatments are needed to achieve good clinical and functional outcomes and to avoid central nervous system complications.
Keywords: Acute retinal necrosis; Herpes virus; Triamcinolone; Valgancyclovir; Cytomegalovirus.
Necrosis retiniana aguda: Informe de un caso
RESUMEN
Objetivo: Describir un caso de necrosis retiniana aguda, las características clínicas, el enfoque diagnóstico y la respuesta al tratamiento.
Método: Se realiza un estudio descriptivo, retrospectivo tipo informe de caso en un paciente de sexo masculino, 26 años de edad, que consulta al Servicio de Urgencias con historia de pérdida visual del ojo derecho (OD) de 3 días de evolución. Al examen de ingreso se encontró una agudeza visual del OD de movimiento de manos y defecto pupilar aferente, y 20/15 en el ojo izquierdo (OI). En el estudio del fondo de ojo derecho se encontraron exudados blandos abundantes y hemorragias que comprometen todo el polo posterior, la hemirretina inferior y la periferia supero temporal. En los exámenes para clínicos se evidenciaron serologías positivas para herpes tipo 1 y 2 en ausencia de VIH y a la angiografía con fluoresceína cambios vasculares con zonas de no perfusión. Se llega al diagnóstico de necrosis retiniana aguda y se decide manejar con valganciclovir endovenoso durante dos semanas, triamcinolona intravítrea y fotocoagulación retiniana con laser para el manejo de la vasculitis severa y zonas isquémicas; luego se continuó con antivirales orales por 3 meses.
Resultados: Después de 2 meses y medio de seguimiento, hay una agudeza visual de 20/50 del OD, un examen biomicroscópico normal, presión intraocular de 12 mm Hg y el fondo de ojo muestra mejoría del cuadro al compararlo con las fotos iniciales.
Conclusiones: Al diagnóstico de NRA se llega con la sospecha clínica, de acuerdo con los signos del examen; se requiere un manejo endovenoso e intravítreo oportuno, para lograr buenos resultados tanto clínicos como funcionales y evitar complicaciones a nivel del sistema nervioso central.
Palabras clave: Necrosis retiniana aguda; Herpes virus; Triamcinolona; Valganciclovir.
Acute retinal necrosis, ARN, is a rather infrequent entity, characterized by retinitis, vasculitis, hemorrhages and areas of retinal necrosis associated to uveitis and optic neuritis, which is not restricted to immune compromised people1. The importance of a sudden suspicion and a quick treatment resides in the lesion aggressiveness transferring into very severe visual sequelae not reversible than can move toward blindness2. Since there is a growing extent of immune depressive patients, absence of this criterion should not be a factor to discard the diagnostic impression. In this paper a case of ARN in a healthy young man with a very aggressive retinal lesion of his right eye is presented.
Clinical report
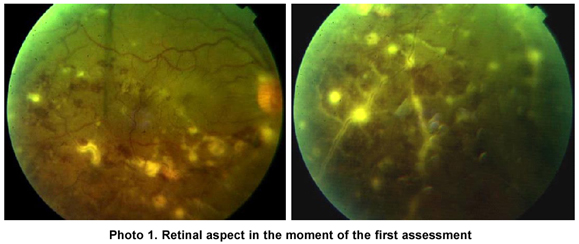
Male patient, 26 years old, who arrives to the Ophthalmology Service (Emergency) with a history of acute vision loss in his right eye and an evolution of three days. At initial exam right eye vision acuity of hands movement with an afferent papillary defect of 3+/4+ and 20/15 in left eye are found. Ocular fundus study discloses vascular changes with abundant soft exudates compromising posterior pole, half inferior of the retina as well as its super-temporal periphery (Photo 1).
Through the eye fundus findings an initial diagnostic impression of right eye cytomegalovirus retinitis was done. In order to confirm the diagnosis a series of para clinic laboratory exams were ordered. Results were negative for HIV, VDRL, IgG and IgM for cytomegalovirus and toxoplasma, but IgG positive for herpes virus 1 and 2 with negative IgM.
According to these results, and since it is well known that infectious processes in their initial phase do not increase IgM, the diagnostic possibility of acute retinal necrosis is planned and a consultation to Infectious Service was made. This service agrees with the diagnosis. The patient is hospitalized and treatment with intravenous valgancyclovir during two weeks is begun and later per os until completing three months. Furthermore, and in accordance with American Academy of Ophthalmology guide lines intra-vitreous triamcinolone was injected for managing the severe vasculitis because the clinical picture has been impaired from its initial aspect. Angiographic study shows a picture of peripheral ischemia associated with vasculitis (Photo 2) and to treat this condition laser photocoagulation is done in ischemic areas. An apparatus of argon laser (Zeiss) with a 200 ìm spot, 120 mV of power, 400 ms interval and 110 ms of duration is used for applying 460 shots in total, with 200 ìm of space between each shot, on ischemic zones in order to avoid the neo vascularization process.
After 2.5 months of follow up patient’s evolution vision acuity of 20/50 to the right eye is found, a bio-microscopic study indicates a clear cornea, anterior segment transparent without inflammatory signs, a central round pupil that dilates to 8 mm, crystalline lens transparent, syneretic vitreous with white cells 1+/4+, eyelids and conjunctivae normal. There is an improvement of ocular fundus when compared to initial photo; optic disc is slightly pale, there is a notorious re-absorption of hemorrhages, macula lutea with inferior perifoveal exudation is less than 500 ìm of diameter (Photo 3).
DISCUSSION
ARN is a very rare syndrome that usually is like a severe vaso-occlusive retinitis, in most of the cases it is unilateral, but around 35% may be bilateral in its development, generally in the first six weeks3. Among ARN diagnostic criteria there are defined focal areas in peripheral retina with necrosis and a circumferential progression of lesions that occur rapidly and progress to occlusive vasculitis. Obviously, if there is no appropriate treatment, either an anterior or posterior uveitis with optic neuritis and retinal detachment should be the results. Associated factors to bad visual prognosis in ARN are, diffuse retinal arteritis, retinal detachment and arterial occlusion. From literature it is also known a multi focused dotted pattern with a very bad prognosis5.
Initially ARN was thought to be present only in immunocompetent people but due to AIDS pandemic and immunosuppressive therapy in transplanted patients, multiple cases in immunocompromised persons have been reported3.
Among ARN etiologic agents several members of herpes virus family have been found. Have been identified zoster smallpox virus, simplex herpes virus types 1 and 2, as well as cytomegalovirus and more rarely Epstein-Barr virus3 Most of the cases of ARN have been described among adult people, more frequently over 25 year old, with simplex herpes virus type 1 and zoster smallpox virus; the first one is related to encephalitic personal history4.
ARN diagnosis is accomplished through the clinical suspicion in accordance with a set of symptoms found. Identification requires opportune intravenous and intra-vitreous management. With a very small sample of aqueous or vitreous humor it is possible to identify etiological agents through the polymerase chain reaction (PCR) which recognizes the viral type. Differential diagnoses include presentations of atypical retinal necrosis due either to toxoplasma, syphilis or ocular lymphoma.
Although diagnosis may be precise with the mentioned techniques, to be ignorant of the disease retards its treatment and diminishes the possibilities of good results in visual acuity and increases the probabilities of neurological complications. Since almost all of the viruses are sensible to acyclovir the therapy must be initiated in the moment of the diagnostic impression; if cytomegalovirus in an immunosuppressant patient is identified, acyclovir can be replaced by gancyclovir. Among other alternatives of antiviral management, foscarnet, brivudine, famcyclovir or valgancyclovir are present. The prophylactic laser barrier in the first two weeks has been used to prevent rheumatic retinal detachment with good results; it can be associated with steroids in severe inflammatory processes.
Interest conflict. The authors declare that there are no interest conflicts in this manuscript.
REFERENCES
1. Chau TH , Stanescu D, Caspers-Velu L, Rozemberg F, Liesnard C, Gaudric A, et al. Clinical characteristics of acute HSV-2 retinal necrosis. Am J Ophthalmol. 2004; 137: 872-9.
2. Lau CH, Missotten T, Salzmann J, Lightman SL. Acute retinal necrosis. Features, management, and outcomes. Ophthalmology. 2007; 114: 756-62.
3. Walters G, James TE. Viral causes of the acute retinal necrosis syndrome. Curr Opin Ophthalmol. 2001; 12: 191-5.
4. Aizman A. Treatment of acute retinal necrosis syndrome. Drugs Today (Barc) 2006; 42: 545-51.
5. Van Gelder RN, Willig JL, Holland GN, Kaplan HJ. Herpes simplex virus type 2 as a cause of acute retinal necrosis syndrome in young patients. Ophthalmology. 2001; 108:869-76.