Adverse drug reactions in internal medicine units at a university hospital: A descriptive pilot study
Luis Carlos López1, Marcela Botero1, Jaime Pino1, Jorge Hernán Ramírez, MD, MSc2, Mauricio Palacios, MD, MSc2
1. Medical student, School of Medicine, Universidad del Valle, Cali, Colombia. e-mail: luis_carlos_lopez@hotmail.com matcheo@hotmail.com jaerpico@yahoo.es
2. Director Programa de Medicina. Facultad de Ciencias de la Salud. Universidad Icesi, Cali, Colombia.
3. Assistant Professor, Department of Physiological Sciences, School of Medicine, Universidad del Valle, Cali, Colombia.
e-mail: jhramirez@icesi.edu.co maopalacios@yahoo.com
Received for publication June 25, 2007 Accepted for publication January 12th, 2010
SUMMARY
Introduction: Adverse drug reactions (ADRs) are an important cause of morbidity and mortality among hospitalized patients.
Objectives: This study was designed to describe the frequency, severity, and causality of ADRs in internal medicine units at a third-level university hospital.
Materials and methods: A descriptive study was performed at internal medicine units, by means of a structured format, review of clinical records, and interview of hospitalized patients. The Naranjo algorithm was applied to patient adverse events to define causality. Additionally, ADRs were classified according to the Rawlins and Thompson criteria.
Results: One hundred patients (50 men and 50 women) were included in the study. Ninety nine (99) adverse events were found among the patients. The Naranjo algorithm was applied to adverse events, resulting in twenty nine (29) probable ADRs, twenty (20) possible ADRs and fifty (50) doubtful ADRs. Cardiovascular drugs and antibiotics were the most frequent therapeutic groups associated with ADRs. In addition, two preventable medication errors were identified.
Conclusions: Frequency of ADRs was similar to the number reported in other studies in internal medicine units. It is necessary to systematize efforts of pharmacological surveillance in hospital wards, toward an opportune detection and prevention of ADRs.
Keywords: Adverse drug reactions; Pharmacological surveillance; Hospitalized patients.
Reacciones adversas a medicamentos en salas de medicina interna de un hospital universitario: Estudio descriptivo piloto
RESUMEN
Introducción: Las reacciones adversas a medicamentos (RAM) son una importante causa de morbilidad y mortalidad en pacientes hospitalizados.
Objetivos: Este estudio se diseñó para describir la frecuencia, severidad y causalidad de las RAM en las salas de Medicina Interna de un hospital universitario de tercer nivel.
Materiales y métodos: Se realizó un estudio descriptivo en las salas de hospitalización de Medicina Interna, con un formato estructurado, revisión de historia clínica y entrevista a los pacientes. Para definir causalidad, se aplicó el algoritmo de Naranjo a los eventos adversos de los enfermos. Además, se clasificaron las RAM de acuerdo con los criterios de Rawlins y Thompson.
Resultados: En el estudio se incluyeron 100 pacientes (50 hombres y 50 mujeres). Se informaron 99 sucesos adversos; con el algoritmo de Naranjo se clasificaron como RAM probables (n=29), RAM posibles (n=21) y RAM dudosos (n=49). Los medicamentos cardiovasculares y los antibióticos fueron los grupos terapéuticos más relacionados con efectos adversos. Se descubrieron dos errores de medicación prevenibles.
Conclusiones: La frecuencia que se encontró de estas reacciones adversas fue similar a la que informaron otras investigaciones en servicios de Medicina Interna. Es necesario sistematizar los esfuerzos de fármaco-vigilancia hospitalaria para prevenir y evitar oportunamente las RAM.
Palabras clave: Farmacovigilancia; Reacciones adversas a medicamentos; Pacientes hospitalizados.
The World Health Organization (WHO) defines adverse drug reactions (ADRs) as «any harmful or undesired response to a medication, occurring at doses used for prophylaxis, diagnosis, and treatment in humans»1. In the United States, ADRs were classified between the fourth and sixth cause of death in 1994, after cardiovascular disease, cancer, accidents, and violence2.
The significant increase of medications commercially available in recent years has generated numerous epidemiological studies aimed at determining the severity, incidence, and direct and indirect costs of ADRs in hospital and ambulatory settings. In hospitalized patients prevalence of ADRs has been reported ranging from 1.2% to 45%, the broad variability of prevalence reported in studies is due primarily to methodological differences in the collection of data and in the use of non-standardized criteria to diagnose the presence of adverse effects to medications2-4. Most research in detecting ADRs has been undertaken in the USA and Europe, with insufficient data on adverse effects in populations in Latin American nations.
Some studies in Latin America have been developed to investigate ADRs. Recently, Tribiño et al., reported an incidence of 25.1% of adverse effects in hospitalized patients in internal medicine wards at a third-level hospital in Bogotá, finding that patients with ADRs presented greater hospitalization stays that directly or indirectly increased hospital costs5. In Brazil, a cohort study reported that 43% of hospitalized patients displayed adverse reactions to at least one medication in third-level internal medicine wards6. The high frequency of ADRs in internal medicine wards is due mainly because patients are usually elderly, have multiple chronic illnesses, and are treated with more than two medications (polypharmacy), placing them at higher risk of adverse effects and drug-drug and drug-illness interactions7-9.
In Colombia and in other Latin American nations, the prevalence, incidence, and mortality of ADRs in hospitalized patients is unknown, in part because of the lack of pharmacological surveillance studies and insufficient reporting of adverse events to the Instituto Nacional de Vigilancia de Medicamentos y Alimentos (INVIMA) [National Institute of Food and Drug Surveillance]. This study was conducted to describe the incidence and the clinical characteristics of the ADRs in internal medicine hospital wards at a university hospital. Additionally, the groups of medications most frequently associated to ADRs were identified, along with the severity of the adverse reactions, potentially preventable adverse effects, and unfavorable drug-drug and drug-illness interactions.
MATERIALS AND METHODS
Population of study. A descriptive study was done at a third-level university hospital located in Cali, Colombia. The hospital has a total of 698 beds, of which 59 correspond to the internal medicine hospitalization service. The study randomly included patients over 18 years of age from both sexes, admitted to the service of internal medicine wards during June, July, and August 2006. Patients who did not present indications of ADRs at admission were included, and who accepted participating in the study; excluding those who revealed communication difficulties, confused or disoriented patients on neurological examination, patients transferred from other hospitalization services, and those who refused to participate in the study.
Based on the data prior to admission to the ward from the previous year (785 men and 824 women), the average monthly admission (65.4 and 68.6, respectively), and the expected incidence of ADRs of 25%; a sample of 140 patients was calculated. At the end of three months of data collection, 40 patients were excluded because they presented at least one of the exclusion criteria, resulting in a total study population of 100 patients, 50 in the male ward and 50 in the female ward.
This project was approved by the Committee of Human Ethics of the Faculty of Health at Universidad del Valle (act Nº 04 of 2006) and by the Ethics Committee at the University Hospital (24 May 2006).
Data collection. Data was gathered via a format designed to detect ADRs. The form was filled out through a semi-structured interview of the patient, review of the medical history, and direct communication with medical personnel rotating in the ward. The form included the following data: 1. Identification of the patient; 2. Current diagnosis and at time of admission to the internal medicine ward; 3. Symptoms presented during hospitalization, including date of onset; 4. Laboratory exams; 5. Medications used before and during the hospitalization.
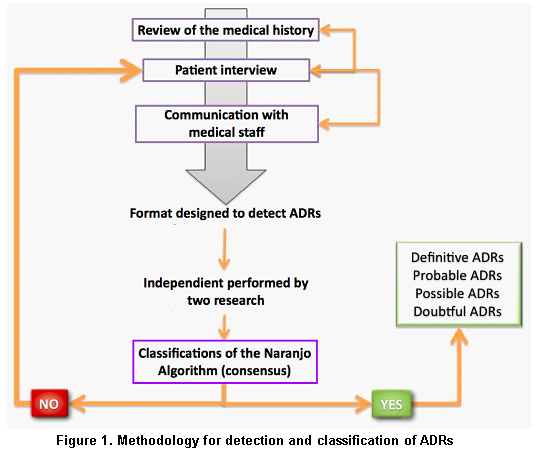
Data analysis. The medications were catalogued according to the Anatomical Therapeutic Chemical (ATC) classification. The International Statistical Classification of Diseases and Related Problems (ICD-10) was employed to classify diseases. The symptoms, signs, and laboratory findings obtained for each patient were evaluated with the Naranjo algorithm to determine causality between the drug and the adverse event presented10. For definition purposes of adverse drug reaction, only adverse events classified as definite, probable, and possible were defined with respect to the administering of a medication. The Naranjo algorithm was independently performed by two researchers (JR, MP). In cases of patients where a classification different to ADRs was found by the two evaluators, the format was and the medical history were again reviewed, and a new interview was given to the patient to determine by consensus the presence or absence of ADRs (Figure 1).
The classification of adverse reactions was done according to the Rawlins and Thompson criteria in categories A and B9. The categorization is done according to the severity of the adverse reaction, the predictability according to the action mechanism of the drug, the relationship with the dose, the duration of the treatment, and the time transpired for the appearance of the adverse effect after administering the medication. The determination of the preventable adverse effects and the classification of the severity was fulfilled as previously described by Dormann et al.11,12.
RESULTS
The study included 100 patients, of which 50 were male and 50 were female with average age of 42.95 years (IC 95% ± 13.41). The hospital stay at the internal medicine ward for the sample was 10.07 (IC 95% ± 7.2), with an average of medications administered of 7.77 (IC 95% ± 2.9). The first five causes of hospitalization correspond to cardiovascular disease (HTA, 25%; acute coronary disease, 12%; and heart failure, 10%), chronic renal insufficiency (16%), and AIDS (12%). The groups of medications prescribed most were cardiovascular drugs and analgesics. In the study, 99 adverse events were identified related to medications in 45 patients (IC 95%, 35.1-54.9), corresponding to probable ADRs (n=29), possible ADRs (n=21), and doubtful ADRs (n=49), after applying the Naranjo algorithm. None of the adverse events was classified as definite. Additionally, doubtful ADRs were not considered adverse effects to medications. In five patients, two ADR events were present simultaneously.
The cardiovascular medications are associated with the greatest number of adverse effects. Of these, enalapril caused the greatest ADRs, consisting of dry cough (n=9), coetaneous rash (n=1), and pharmacological interactions with other cardiovascular medications (n=2), followed by amlodipine (n=8), furosemide (n=6), clindamycin (n=4), lovastatin (n=3), and ceftriaxone (n=3). All ADRs associated with enalapril were catalogued as slight. Other cardiovascular medications related to ADRs were amlodipine and furosemide that mainly caused palpitations and orthostatic hypotension (n=12). Additionally, the antilipemic lovastatin was associated to myalgia in three patients. The second group of medications most frequently linked to ADRs was antibiotics, primarily clindamycin and ceftriaxone, both associated with diarrhea and coetaneous rash.
According to the classification by Rawlins and Thompson, 92% of the ADRs found in the Ward were classified as type A adverse effects (dose dependent, predictable, common) and the remaining 8% were classified as type B (dose independent, unpredictable, uncommon). All the type B adverse effects described in the ward corresponded to maculopapular rash related with the administering of clindamycin (3 patients) and ceftriaxone (1 patient).
Adverse reactions were also classified by systems (Table 1). The system where the greatest number of ADRs was the gastrointestinal system, present in 36% of all the cases, which consisted mainly of nausea and vomit (8 patients) secondary to the administering of opioids, antineoplastics, and antibiotics. Five patients presented diarrhea secondary to the use of antibiotics and in four patients constipation was associated to the administering of opioids, tricyclic antidepressants, and antacids. Joint administering of acetylsalicylic acid and clopidogrel caused melenas in one patient.
Other systems commonly affected by ADRs were the cardiovascular system (orthostatic hypotension and palpitations by antihypertensives), the respiratory system (cough secondary to IECAs), the skin (rash secondary to antibiotics and IECAs) and the muculoskeletal system (myalgia secondary to Statins). Only two cases were detected of adverse effects in the hydroelectrolitic balance, both related to hypokalemia because of diuretics. In the central nervous system, the study detected one case of sedation related to the use of pregabalin. No hematologic (anemia, thrombocytopemia, neutropenia), hepatic (hepatoxicity), or renal (nephrotoxicity) adverse effects were detected secondary to the use of medications in the ward.
Thirteen adverse reactions were identified related to the simultaneous use of two or more medications. Six patients presented orthostatic hypotension and palpitations caused by the combination of antihypertensive medications; primarily the simultaneous use of vasodilators and diuretics. In four patients, diarrhea was related to the simultaneous use of two antibiotics. In one asthmatic patient with cardiac insufficiency, the study detected hypokalemia secondary to the administering of furosemide and b2 agonists, which was diagnosed and treated opportunely. The rest of the adverse effects related to drug interactions are described in Table 2.
A case was identified with errors in the administration of the medication, corresponding to the irregular administering of clonidine, without presenting significant variations in blood pressure and one case of medication combination requiring close monitoring, which consisted in the concomitant use of genfibrozil with lovastatin without evidencing myalgia or other signs that would indicate the presence of rhabdomyolysis in this patient.
DISCUSSION
In the current study, a descriptive analysis was performed of the adverse reactions to medications at an internal medicine service. In gathering the data, we were aware that the medical history could have incomplete information; hence, the medications prescribed to each patient (presentation, dose, and route of administration) were confirmed by the format of medication administration used by nursing personnel and by the physicians responsible for the ward. In spite of the limitation in collecting data through the medical history, previous studies of pharmacological surveillance have described a high correlation between medications administered to patients and those registered in the medical history13.
Active pharmacological surveillance in hospital settings presents multiple advantages with respect to programs of voluntary notification of adverse effects. The strategy for detecting adverse effects applied in this study permits obtaining complete information of the patientís illness and the drugs administered. Additionally, this methodology permits checking the veracity of the data related to the administration of the medication (dose, commercial presentation, route of administration, date of prescription) indispensible in determining if there is or isnít causality of an adverse effect. This system of pharmacological surveillance is low cost and can be easily applied in hospitalization services in Latin American nations to increase the prevention and early detection of adverse effects in hospitalized patients14.
This study did not detect serious adverse effects in patients hospitalized in the internal medicine ward; this is only explained in part by some limitations of the methodology. In the first place, simple size is insufficient to detect serious adverse effects, given that it was calculated based on a 25% frequency of all types of ADRs and not based on the frequency estimated of 1 to 2% of serious ADRs. In the second place, the study did not conduct follow up of the patients, which could diminish detecting infrequent ADRs.
Cough secondary to the use of enalapril was the most common adverse effect related to an individual drug. This can be explained because cough occurs in 20 to 30% of the individuals who consume Inhibitors of Angiotensin Converting Enzyme (IACEs), and 29% of the patients in the ward were being treated with enalapril15,16. The high frequency of orthostatic hypotension associated to the use of antihypertensives may be due to the characteristics of the patients in the ward, where the most frequent diagnoses are cardiovascular diseases like hypertension, cardiac insufficiency, and acute myocardial infarction.
It is necessary to conduct studies with a greater number of patients to determine preventable risks with the use of medications in internal medicine hospitalization services, since the current study found two situations that are potentially related with adverse reactions, that if they were to occur they could be classified as serious or severe. These efforts should be frame worked within an ordered program of pharmacological surveillance, which should be organized foremost in compliance with Decree 2200 of 2005 from the Ministry of Social Protection and from the responsibility of this being a teaching institution, which brings challenges as well as advantages in its introduction.
ACKNOWLEDGMENTS
The authors wish to thank the patients who participated in this study and the internal medicine hospitalization personnel at Hospital Universitario del Valle, headed by Doctor Lena Barrera, Unit director.
Conflict of interest. None of the authors has conflicts of interest related to this study.
REFERENCES
1. World Health Organization. Safety of medicines: a guide to detecting and reporting adverse drug reaction. Geneva: WHO; 2002.
2. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998; 279: 1200-5.
3. Hazell L, Shakir SA. Under-reporting of adverse drug reactions: a systematic review. Drug Saf. 2006; 29: 385-96.
4. Kvasz M, Allen IE, Gordon MJ, Ro EY, Estok R, Olkin I et al. Adverse drug reactions in hospitalized patients: A critique of a meta-analysis. MedGenMed. 2000; 2: E3.
5. Tribino G, Maldonado C, Segura O, Díaz J. Direct costs and clinical aspects of adverse drug reactions in patients admitted to a level 3 hospital internal medicine ward. Biomedica. 2006; 26: 31-41.
6. Camargo AL, Cardoso Ferreira MB, Heineck I. Adverse drug reactions: a cohort study in internal medicine units at a university hospital. Eur J Clin Pharmacol. 2006; 62: 143-9.
7. Tavassoli N, Bagheri H, Sailler L, Benkemoun P, Montastruc JL, Arlet P. Estimation of time devoted to adverse drug reactions assessment in an internal medicine department. Br J Clin Pharmacol. 2005; 60: 452-3.
8. Callreus T. Use of the dose, time, susceptibility (DoTS) classification scheme for adverse drug reactions in pharmacovigilance planning. Drug Saf. 2006; 29: 557-66.
9. Edwards IR, Aronson JK. Adverse drug reactions: definitions, diagnosis, and management. Lancet 2000; 356: 1255-9.
10. Naranjo CA, Shear NH, Lanctot KL. Advances in the diagnosis of adverse drug reactions. J Clin Pharmacol. 1992; 32: 897-904.
11. Dormann H, Neubert A, Criegee-Rieck M, Egger T, Radespiel-Troger M, Zaz-Livshits T et al. Readmissions and adverse drug reactions in internal medicine: the economic impact. J Intern Med. 2004; 255: 653-63.
12. Dormann H, Muth-Selbach U, Krebs S, Criegee-Rieck M, Tegeder I, Schneider HT et al. Incidence and costs of adverse Andrug reactions during hospitalisation: computerised monitoring versus stimulated spontaneous reporting. Drug Saf. 2000; 22: 161-8.
13. Heineck I, Ferreira MBC, Doering PL, Schenkel E. Accuracy of medical records in documenting drug therapy in routine surgical procedures. Hosp Pharm. 1999; 34: 946-8.
14. Laporte JR, Tognoni G. Farmacovigilancia en el hospital. En: Principios de epidemiologia del medicamento. Madrid: Ediciones Científicas y Técnicas SA; 1993. p. 21 9-31.
15. Tomlinson B, Woo J, Thomas GN, Chau YM, Critchley JA. Randomized, controlled, parallel-group comparison of ambulatory and clinic blood pressure responses to amlodipine or enalapril during and after treatment in adult chinese patients with hypertension. Clin Ther. 2004; 26: 1292-304.
16. Tumanan-Mendoza BA, Dans AL, Villacin LL, Mendoza VL, Rellama-Black S, Bartolome M et al. Dechallenge and rechallenge method showed different incidences of cough among four ACE-Is. J Clin Epidemiol. 2007; 60: 547-53.