Bee sting of the cornea. Case report
Mauricio Vélez, MD1, Gloria I. Salazar, MD2, Patricia Monsalve, MD2
1. Cornea Professor, Department of Ophthalmology, Universidad Pontificia Bolivariana, Medellín, Colombia.
e-mail: mauroftalmo@hotmail.com
2. Medical Resident of Ophthalmology, Department of Ophthalmology, Universidad Pontificia Bolivariana, Medellín, Colombia. e-mails: atabel@hotmail.com monsalve81@hotmail.com
Received for publication July 23, 2009 Accepted for publication March 10, 2010
SUMMARY
Bee stings of the eye are uncommon entities and ocular reactions to the bee venom are wide, ranging from mild conjunctivitis to sudden vision loss. We present the case of a patient who suffered a bee sting of the cornea and the response to the poison components. We go through the bee venom properties, its actual treatment, and propose a new management alternative.
Keywords: Cornea; Bee venom; Triple procedure.
Picadura de abeja en la córnea. Informe de un caso
RESUMEN
Las picaduras de abeja en el ojo son entidades poco comunes y las reacciones oculares al veneno de abeja son amplias, pues van desde una leve conjuntivitis hasta la pérdida aguda de la visión. Se presenta el caso de un paciente que sufrió la picadura de una abeja en la córnea y la respuesta frente a los componentes de este veneno. Se realizó una revisión de las propiedades del veneno de abeja, su tratamiento actual y se propone una nueva alternativa de manejo.
Palabras clave: Córnea; Veneno de abeja; Triple procedimiento.
Bees are insects that belong to the Hymenoptera order, they have a real stinger that stays attached to the tissue, dragging with itself the venom glands. The poison is a complex mixture of toxic substances as phospholipase A, melittin, apamine, hyaluronidase and mast cell degranulating peptide (MCD) among others1. The corneal bee sting is a rare event and injuries associated with it can appear as penetrating, immunologic, or toxic presentations; or as a combination of all three mechanisms. These lesions are more related with the local effect of the poison, than with the presence of the sting itself2. In the literature we find a wide spectrum of ocular manifestations, which includes: corneal edema, corneal infiltration, chemosis, ciliary injection, mucopurulent keratoconjunctivitis, anterior uveitis, hyphema, iris atrophy, cataract, lens subluxation, anterior and posterior capsule opacities, trabeculitis, damage of the trabecular mesh and glaucoma, ophthalmoplegia, optic neuritis, papilledema and optic atrophy3,4.
We present the case of a patient with a bee sting in cornea without retention of the stinger, who developed corneal decompensation and opacification of the lens as a side effect of the poison. Pathophysiologic mechanisms involved in these injuries will be discussed and therapeutic alternatives will be proposed.
CASE REPORT
A 60 year-old man, presented to cornea consultation, looking for improvement in his vision. As an important antecedent, the patient related having had a bee sting to the left eye 6 months before presentation. In the first centre where he was handled, he received an ocular surface wash and was prescribed with prophylactic antibiotics and corticosteroids (without detailed information about the medicines and their doses). Since then, he relates having lost visual acuity in that eye.
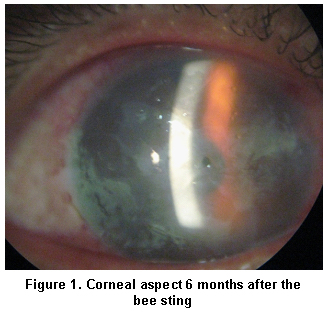
Visual acuity was counting fingers 1 meter which did not improve with pinhole, slit-lamp examination showed a completely opaque cornea with superficial neovascularization compromising one of its quadrants, this opacity did not allow appreciation of anterior segment details (Figure 1). Eye movements were clinically normal and intraocular pressure was 15 mm Hg in both eyes.
An ocular ultrasound reported an ecosilent vitreous cavity, the retino-choroideal complex had normal aspect, no increase in the optic nerve cup was found but a dense cataract was evidenced (Figure 2).
It was decided to perform a triple procedure including penetrating keratoplasty, cataract extraction and intraocular lens implantation, with successful evolution, achieving a non-corrected visual acuity of 20/100 (Figure 3).
DISCUSSION
The bee venom is a complex mixture of chemicals with toxic activities. Phospholipase A and melittin represent 75% of the venom components. Phospholipase A acts on the red blood cells membrane causing haemolysis and over other cells causing disruption of their membranes and release of potassium and biogenic amines (such as histamine and dopamine). Melittin and MCD peptide produce mastolisis, histamine and serotonin release, edema and pain. Apamin acts as a motor action neurotoxin which alters neurotransmission by blocking potassium channels1,2.
It has been proposed that conjunctival injection, conjunctival chemosis and corneal edema may be due to a Type 1 hypersensitivity reaction (mediated by IgE) to the enzymes in the venom. Hyphema may be due to the haemolytic effect of phospholipase A and lysolecithin. Hyaluronidase, hemolitin, minimine and other amines of the venom may cause degeneration and lysis of the chromophores leading to iris despigmentation4.
The apamin has been implicated in the development of ophthalmoplegia (secondary to neuroparalysis of the third cranial nerve), iridoplegia, optic neuritis, papilledema and optic atrophy2. It has been proposed that optic neuropathy associated with bee sting, is due to acute demyelization of the optic nerve5, however the exact mechanism for this event is unknown. Melittin may be responsible for generated changes in the lens since it reduces the conformational order of proteins and interacts with lipids breaking their structure; these changes lead to loss of lens transparency and to its irreversible opacification6.
Treatment reported in literature for the management of corneal bee stings can be divided into acute and long-term measures. Acute measures include:
Steroids use to reduce inflammation induced by the poison. Topical antibiotics to prevent secondary infection. Oral anti-histamines to counteract the activity of biogenic amines 4. Cycloplegics to relieve pain from ciliary spasm and prevent synechiae formation. Surgical removal of the sting. The use of paracentesis in severe iritis with hypopyon has been described, especially when the sting has penetrated the anterior chamber4.
Long-term management includes: refractive correction of the astigmatism generated by a corneal scar, penetrating keratoplasty when the scar compromises the visual axis directly or when there is corneal decompensation due to endothelial cell damage, and cataract surgery if required4.
In the reported case, we found a patient 6 months after a bee sting, who even without presenting stinger retention, suffered from complications associated with the toxic effect of the venom (corneal decompensation and cataract development) which required aggressive measures for correction (penetrating keratoplasty and cataract surgery). Our team work proposal is to perform early washing of the anterior chamber with balanced salt solution, associated with subconjunctival corticosteroid injection (ideally within the first 24 hours) and systemic treatment with methylprednisolone (500 mg intravenously every 6 hours during 3 days) to avoid the deleterious effects that poison can cause in the eye, and all the possible complications derived from there.
REFERENCES
1. Córdoba D. Toxicología. 5a ed. Bogotá, DC: Ed. Manual Moderno; 2006. p. 673-5.
2. Smith DG, Roberge RJ. Corneal bee sting with retained stinger. J Emerg Med. 2001; 20: 125-8.
3. Jain V, Shome D, Natarajan S. Corneal bee sting misdiagnosed as viral keratitis. Cornea. 2007; 26: 1277-8.
4. Chuah G, Law E, Chan WK, Ang CL. Case reports and mini review of bee stings of the cornea. Singapore Med J. 1996; 37: 389-91.
5. Maltzman JS, Lee AG, Miller NR. Optic neuropathy occurring after bee and wasp sting. Ophthalmology. 2000; 107: 193-5.
6. Ghosh SK, Chattopadhyay D, Senz AC, Chakrabarti B. Melitin-induced conformational changes in human lens protein. Curr Eye Res. 1991; 10: 1065-8.