Latissimus dorsi transposition for sequelae of obstetric palsy
Enrique Vergara-Amador*
*Associate
Professor, Hand surgeon and Pediatric orthopedist, Department of
Orthopedics, Universidad Nacional de Colombia, Bogotá, DC,
Colombia. Ancient resident, Institut Francais de la Main, Paris,
France.
e-mail: emvergaraa@unal.edu.co
Received for publication July 23, 2009 Accepted for publication May 7, 2010
SUMMARY
Background: In
obstetric palsy, limitation in the external abduction and rotation of
the shoulder is the most frequent sequelae. Glenohumeral deformity is
the result of muscular imbalance between the external and internal
rotators. Releasing the contracted muscles and transferring the
latissimus dorsi are the most common surgeries in this case.
Patients and methods: We
operated on 24 children between 4 and 8 years of age with obstetric
palsy sequelae to elevate the subscapularis muscle off the anterior
surface of the scapula posteriorly and transfer the latissimus dorsi.
The patients received a minimum of 2 years of follow up. They were
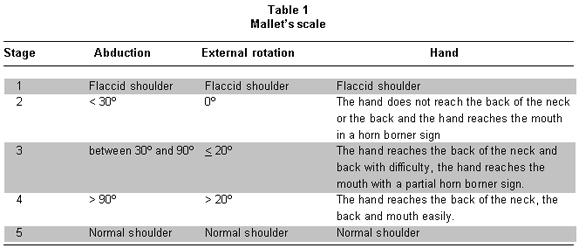
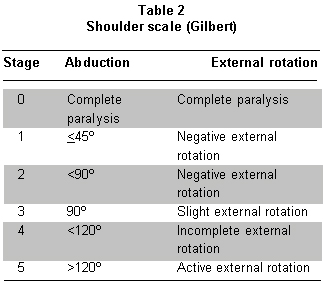
evaluated based on Mallet’s and Gilbert’s classifications.
Results: All of the
patients recovered within the above mentioned classifications. Out of
22 children evaluated via Mallet’s classification, all improved
from 3 to 4 on that scale. With respect to Gilbert’s
classification, 16 children improved one degree and 8 improved 2
degrees. All of the patients’ parents were satisfied with the
results.
Discussion: The benefit
from releasing contracted muscles and muscle transfer to improve
shoulder abduction in the sequelae of obstetric palsy has been amply
reported in the literature. The results we had from elevating the
subscapularis muscle off the anterior surface of the scapula and
transferring the latissimus dorsi were good. Children who were
difficult to classify based on the described scale were taken note of
and some sub-classifications for Gilbert’s descriptions were
proposed. Patients must be selected carefully. To transfer the
latissimus dorsi, it is necessary to have good passive mobility in
abduction, a minimum of 20º of external rotation and no joint
deformities. When negative external rotation is found, the
subscapularis muscle should be released. When there is glenohumeral
joint deformity in older children, other methods are recommended, such
as rotational humeral osteotomy.
Keywords: Obstetric palsy; Transfers muscular shoulder; Latissimus dorsi; Subscapular.
Transferencia del músculo dorsal ancho en secuelas obstétricas del plexo braquial
RESUMEN
Introducción:
Las limitaciones en la abducción y la rotación
externa del hombro son las secuelas más frecuentes en la
parálisis obstétrica. Se encuentra deformidad de la
articulación glenohumeral como resultado del desequilibrio que
existe entre los músculos rotadores externos e internos. Dentro
de las cirugías más usadas para corregir las deformidades
del hombro están las liberaciones musculares y la
transposición del músculo dorsal ancho.
Materiales y métodos: El
autor operó 24 niños entre los 4 y 8 años de
edad, con secuelas de parálisis braquial
obstétrica, a quienes se les practicó liberación
del subescapular por vía posterior y transferencia del
músculo dorsal ancho. Se evaluaron según la escala de
Mallet y la de Gilbert, con un seguimiento mínimo de dos
años.
Resultados: Todos los
niños se recuperaron según las escalas mencionadas. En 22
evaluados según Mallet, todos mejoraron del nivel 3 al 4.
Según la clasificación de Gilbert, 16 niños
mejoraron un grado y 8 niños mejoraron dos grados. Todos los
padres estuvieron satisfechos con los resultados.
Discusión:
Existen muchos informes en la literatura médica sobre los
beneficios de liberar los músculos contracturados y de las
transferencias musculares en el hombro en las secuelas de
parálisis braquial obstétrica. Se obtuvieron buenos
resultados en todos los niños. Algunos casos fueron
difíciles de clasificar en las escalas usadas, para lo cual se
propone una sub-clasificación. Se requiere tener una buena
movilidad pasiva, que no haya deformidad articular en el hombro y
mínimo 20º de rotación externa, para realizar la
transferencia muscular del dorsal ancho. Cuando no se encuentra la
rotación externa, se debe hacer la liberación del
subescapular. Si hay deformidad de la articulación glenohumeral,
no se recomiendan las transferencias musculares y entonces se recurre a
osteotomías.
Palabras clave: Parálisis braquial obstétrica; Transferencia muscular; Dorsal ancho.
In obstetric brachial plexus injuries, most patients recover
spontaneously without surgery. The nerve roots frequently compromised
by typical Erb’s palsy are C5 and C6, where an absence of
abduction and external rotation of the shoulder, flexion of the elbow
and supination of the forearm are found. When the C7 nerve root is
affected, a deficit in the extension of the hand is gene-rally found.
Many of the total injuries at the beginning recovery of the lower
roots and remain a definitely lesion of the upper plexus. Non-recovery
of the bicep flexion against gravity before 3 to 4 months of age or of
the deltoids has been an indication that plexus exploration is necessary1-3.
This indication has been extended to 6-9 months by different authors
who have argued that nerve reconstruction procedures are useful up to
the first year of age4,5. Good functioning is expected for
children who recover anti-gravity biceps strength before the age of 6
months. In the case of children whose biceps recover before the age of
6 weeks, it is possible to achieve total recovery6.
Limitation in abduction and external rotation caused by weakness in the
deltoid muscles and the external rotators of the shoulder are the most
frequent secondary deformities. Contracture in adduction and internal
rotation could appear early due to the lack of opposition to the muscle
forces generated by the subscapularis, pectoralis major, teres major
and latissimus dorsi.
This difficulty in performing external rotation will produce posterior
subluxation of the humeral head in the long term, causing it and the
glenoid to become deformed. This will in turn bring about limitation in
mobility and pain in the long run7,8. Early reconstruction,
along with the release of the contracted tendons and tendinous
transfers, will improve passive and active mobility and retard
deformities in the glenohumeral joint9,10.
Releasing the compromised structures includes elevation of the
subscapularis muscle. This can be done on the tendinous part of the
muscle but it is not generally recommended because of the risk of
residual instability. It can also be done through the posterior
approach by releasing the muscle on the anterior surface of the scapula5,11-13 and releasing the teres major and the pectoral major.
The transfer of the latissimus dorsi muscle is done to improve external
rotation and the abduction at the same time. In 1934, L’Episcopo14 described the transfer of the latissimus dorsi and teres major to the lateral humerus to improve external rotation. Hoffer10
described the transfer of the latissimus dorsi by taking it posterior
and superior in a rotator cuff to allow greater external rotation and
abduction with a functional deltoid. When a good latissimus dorsi does
not exist, transfers of the trapezium or of the scapula elevator may be
considered12,15,16.
The purpose of this article is to describe the results in a case series
with in the transfer of the latissimus dorsi with the elevation of the
subscapularis muscle off the anterior surface of the scapula in
children with obstetric palsy sequelae.
PATIENTS AND METHODS
There were 24 patients with obstetrical brachial plexus sequelae who
had operations performed by the same surgeon (EVA), between 1997 and
2006, to transfer the latissimus dorsi, which, in the cases of 11
children, was associated with elevation of the subscapularis muscle.
There was a minimum follow up of 2 years. Movement of the shoulder was
limited in all cases, especially in abduction and external rotation,
which made it difficult to carry out some ordinary daily activities
like getting dressed, combing the hair, and lifting objects to the face
or mouth. Six patients had an operation on the plexus before they were
one year of age and 18 had not received any surgical treatment.
A transfer of the latissimus dorsi to the infraspinous and supraspinous
tendon was done on all of the patients. Releasing the subscapularis
muscle was done at the same time on 11 patients except for one who had
been operated on at 3 years of age to elevate just the subscapularis
muscle. The criteria for releasing the subscapularis muscle was
external passive rotation of less than 20º. All the patients had
normal morphology in the X-rays. When there was a poor image on the X-
ray, a CT scan was taken. The average age at the time of surgery was
5.1 years of age (ranging from 4 to 8 years of age). The minimum age
for surgery was 4; patients were evaluated before and after the
operation based on Mallet’s scale and the scale for the shoulder
described by Gilbert (Tables 1, 2).
Surgical technique.
The patient is placed in lateral decubitus position under general
anesthesia. An approximately 5 cm axial incision is made on the lateral
border of the scapula when a release of the scapula is being planned.
When only a transfer is planned, the incision is made in the posterior
axillary fold; it is dissected subcutaneously and the interval of the
latissimus dorsi with the teres major is located on the external border
of the scapula. If the latissimus dorsi is of poor quality, the teres
major will be added to the transfer. Because the teres major is
smaller with a lesser excursion than the latissimus dorsi, the teres
major is released from the latissimus dorsi and sutured to the same
muscle more proximally, thus, integrating the two muscles to the
transfer. The dissection towards the humerus is performed with extreme
care. It is not necessary to see the radial nerve. This last part can
be done with blunt dissection up to the insertion of the latissimus
dorsi into the humerus. The muscle is released and lifted while being
careful not to exert tension on the vascular-nervous pedicle. With the
latissimus dorsi lifted, we reach the lateral border of the scapula and
the subscapularis muscle is lifted subperiosteally, starting on the
lateral and inferior border and continuing towards the medial and
superior border with a periosteal elevator. It is important to release
the medial corners because, if not, the subscapularis muscle cannot
slide well. After that, the shoulder should rotate 30º externally.
If it is not possible to achieve good external rotation at the moment,
consider releasing the anterior capsule of the shoulder and of the
coracohumeral ligament (CHL) without cutting the subscapularis muscle
tendon.
The latissimus dorsi tendon goes under the deltoids and it is sutured
to the infraspinous on the lateral superior part. A fast anchor was not
used in any case. If abduction improvement is rendered, the latissimus
dorsi is sutured to the supraspinatus tendon with the arm at maximum
external rotation and an abduction of 90 to 120º. The wound is
closed in two layers with absorbable suture. The arm is immobilized in
a position of minimal abduction of 90º degrees and with external
rotation in the Statue of Liberty position for 5 weeks. When
rehabilitation is started, immobilization is continued at night for
three more weeks.
RESULTS
Overall, we obtained good results; there were no hematomas,
neurological or vascular injuries, nor infection. Of 22 patients scored
on Mallet’s functional scale, all were at 3 points before surgery
and improved to 4 points. Based on Gilbert’s scale, 13 patients
were at 3 before surgery and improved to 4. Seven patients were at 2
and improved to 4. One patient was at an intermediate classification
between 2 and 3 and improved to 4. One patient went from 3 to 5, and
two patients went from 4 to 5. In other words, all of the patients
improved in the two scales (Figures 1, 2; Table 3). The parents of the patients were satisfied with the functional results (Figures 3, 4).
DISCUSSION
External rotation and abduction of the shoulder with progressive
contracture in internal rotation and adduction are the most important
sequelae for the shoulder in obstetric paralysis. The muscular
imbalance between the weak external rotator (infraspinous) and the
strong internal rotators (teres major, latissimus dorsi, pectoral
major, and subscapularis) is the main factor for deformity in internal
rotation and adduction of the shoulder.
The subscapularis is the largest of the four rotator cuff muscles. Einarsson et al.17,
demonstrated the abnormal mechanical properties of the subscapularis
muscle in individuals with obstetric brachial plexus palsy when they
analyzed the passive mechanical characteristics of biopsies from the
subscapularis muscle obtained through open surgery.
Secondary deformities such as the elongation of the coracoids,
flattening or deformation of the humeral head with subluxation or
posterior dislocation and flattening or retroversion of the glenoid may
be found7,8.
Hoeksma et al.7, reported a 56% prevalence of contractures
greater than 10% and a 33% prevalence of osseous deformity in a series
of 53 patients treated without surgery. Waters et al.9, say
that the natural history of obstetrical brachial paralysis with
muscular weakness is glenohumeral deformity because of muscular
imbalance. Using computed tomography (CT) or magnetic resonance imaging
(MRI) to evaluate the gleno scapular angle (retroversion) on a series
of 42 patients, the healthy side showed -5.5 on the average and the
affected side, -25.7 with 62% of the patients presenting posterior
subluxation and increased deformity with age.
Bahm et al.18, noted that although the muscular imbalance
might explain most of the progressing deformities of the glenohumeral
joint, it was necessary to be aware of the rare cases of connatal
traumatic subluxations of the humeral head, which can cause a rapid
contracture requiring immediate surgery.
The anterior release of the subscapularis muscle has been used
extensively but has the drawback of causing anterior instability in the
shoulder. Carlioz and Brahimi11 improved the external
rotation of the shoulder by releasing the subscapularis muscle off the
anterior surface of the scapula through a posterior approach. This is
indicated when the patient still has a congruent glenohumeral joint13,19.
If the external rotator muscles are weak, transfer of the latissimus
dorsi should be done immediately, as well. This transfer will improve
active abduction of the shoulder given that it stabilizes the rotator
cuff and makes the deltoids more effective13,16.
Pagnotta et al.13, evaluated 203 patients who had undergone
operations on their shoulders followed by long-term follow up. This
showed that individuals benefiting most from the surgery were children
who had C5 and C6 paralysis and those who scored 2 and 3 on the Gilbert
scale. According to the authors, six years after the surgery some
patients presented loss of abduction but kept external rotation. It is
possible that the cause of this is functional exclusion on the part of
the child and lack of rehabilitation.
All of the children in this report improved in abduction and external
rotation. Our follow up is relatively short and loss of abduction has
not been observed. All of the children improved on the functional
scales. The 22 who were evaluated based on Mallet’s scale
improved one degree. Eight patients improved two degrees and 16
patients improved one degree based on Gilbert’s scale. Two
children could not be correctly classified on Mallet’s scale
prior to surgery. They had more than 90º of abduction but a
deficit of external rotation of 0º and -20º.
We noticed patients who were not easily classified. There were children
who were found between Mallet’s classifications of 3 and 4. There
were patients whose degrees of abduction were greater than 90º,
but whose external rotations were less than 20º or negative,
making it impossible to classify them. Gilbert’s classification
gives us a closer approach to reality than Mallet’s, although
there are some patients whose recovery of abduction and external
rotation are dissociated. For example, case 16 presented abduction
greater than 120º, but an external rotation of 0º.
Currently, patients who are classified into stages 3, 4, and 5 on
Gilbert‘s scale are being evaluated and sub-classified. The
breakdown we used for this sub-classification is the following:
. 3A: abduction of 90º and external rotation of 0º or negative
. 3B: abduction of 90º and slight or positive external rotation
. 4A: abduction of less than 120º and external rotation of 0º or negative
. 4B: abduction of less than 120º and positive or incomplete external rotation
. 5A: abduction greater than 120º and external rotation less than 20º
. 5B: abduction greater than 120º and external rotation greater than 20º
The patients have to be carefully selected. Good passive mobility in
abduction, a minimum external rotation of 20º and no joint
deformities are required for the transfer of the latissimus dorsi. When
an external rotation of 0º or negative is found, releasing the
subscapularis muscle is considered. At the same time, we evaluated
whether or not it was necessary to release the major pectoral muscle.
Sometimes, though not in this series, it is necessary to release the
anterior capsule of the glenohumeral joint through an anterior approach
or the coracohumeral ligament.
When there is posterior subluxation or glenohumeral joint
deformity in older children, other methods are recommended such as
rotational osteotomy of the proximal humerus20.
No benefits in any form have been received or will be
received from any commercial party related directly or indirectly to
the subject of this article.
REFERENCES
1. Gilbert A, Tassin JL. Surgical repair of the brachial plexus in obstetric paralysis. Chirurgie. 1984; 110: 70-5.
2. Waters PM.
Comparison of the natural history, the outcome of microsurgical repair
and the outcome of operative reconstruction in brachial plexus birth
palsy. J Bone Joint Surg Am. 1999; 81-A: 649-59.
3. Birch R, Ahad N,
Kono H, Smith S. Repair of obstetric brachial plexus palsy: results in
100 children. J Bone Joint Surg (Br). 2005; 87-B: 1089-95.
4. Clarke HM, Curtis
C. Examination and prognosis. In: Gilbert A (ed.). Brachial plexus
injuries. London: Martin Dunitz in association with the Federation of
European Societies for Surgery of the Hand; 2001. p. 159-72.
5. Haerle M, Gilbert A. Management of complete obstetric brachial plexus lesions. J Pediatr Orthop. 2004; 24: 194-200.
6. Waters PM. Update on management of pediatric brachial plexus palsy. J Pediatr Orthop B. 2005; 14: 233-44.
7. Hoeksma AF, Ter
Steeg AM, Dijkstra P, Nelissen RG, Beelen A, Jong BA. Shoulder
contracture and osseous deformity in obstetrical brachial plexus
injuries. J Bone Joint Surg Am. 2003; 85-A: 316-22.
8. Birch, R. Medial
rotation contracture, posterior dislocation of the shoulder. In:
Gilbert A (ed.). Brachial plexus injuries. London: Martin Dunitz in
association with the Federation of European Societies for Surgery of
the Hand; 2001. p. 249-59.
9. Waters PM, Bae DS.
Effect of tendon transfers and extraarticular soft-tissue balancing on
glenohumeral development in brachial plexus birth palsy. J Bone Joint
Surg. 2005; 87-A: 320-5.
10. Hoffer M,
Wickenden R, Roper B. Brachial plexus birth palsies. Results of tendon
transfers to the rotator cuff. J Bone Joint Surg. 1978; 60-A: 691-5.
11. Carlioz H, Brahimi
L. La place de la désinsertion interne du sous-scapulaire dans
la traitement de la paralysie obstétricale du membre
supérieur chez l’enfant. Ann Chir Infantile. 1971; 12:
159-67.
12. Raimondi PL, Muse
A, Saporiti E. Palliative surgery: shoulder paralysis. In: Gilbert A
(ed.). Brachial plexus injuries. London: Martin Dunitz in association
with the Federation of European Societies for Surgery of the Hand;
2001. p. 225-38.
13. Pagnotta A, Haerle
M, Gilbert A. Long-term results on abduction and external rotation of
the shoulder after latissimus dorsi transfer for sequelae of obstetric
palsy. Clin Orthop Relat Res. 2004; 426: 199-205.
14. Strecker WB,
McAllister JW, Manske PR, SchoeneckerPL, Dailey LA.
Sever-L’Episcopo transfers in obstetrical palsy: a retrospective
review of twenty cases. J Pediatr Orthop. 1990; 10: 442-4.
15. Chen L, Gu YD, Hu
SN. Applying transfer of trapezius and/or latissimus dorsi with teres
major for reconstruction of abduction and external rotation of the
shoulder in obstetrical brachial plexus palsy. J Reconstr Microsurg.
2002; 18: 275-80.
16. Van Kooten EO,
Fortuin S, Winters HA, Ritt MJ, Van der Sluijs HA. Results of
latissimus dorsi transfer in obstetrical brachial plexus injury. Tech
Hand Up Extrem Surg. 2008; 12: 195-9.
17. Einarsson F,
Hultgren T, Ljung BO, Runesson E, Fridén J. Subescapularis
muscle mechanics in children with obstetric brachial plexus palsy. J
Hand Surg Eur. 2008; 33: 507-12.
18. Bahm J, Wein B,
Alhares G, Dogan C, Radermacher K, Schuind F. Assessment and treatment
of glenohumeral joint deformities in children suffering from upper
obstetric brachial plexus palsy. J Pediatr Orthop (Br). 2007; 16:
243-51.
19. Gilbert A. Long-term evaluation of brachial plexus surgery in obstetrical palsy. Hand Clin. 1995; 11: 583-95.
20. Kirkos JM,
Papadopoulos IA. Late treatment of brachial plexus palsy secondary to
birth injuries: rotational osteotomy of the proximal part of the
humerus. J Bone Joint Surg. 1998; 80-A: 1477-83.
|