Report of the first case of myxoid liposarcoma in Colombia: a rare tumor
Luz Fernanda Sua, MD*, Nhora María Silva, MD*
* Resident,
Pathological Anatomy and Clinical Pathology, School of Medicine,
Faculty of Health, Universidad del
Valle, Cali,
Colombia. e-mail: lufer24@hotmail.com e-mail: nhorita13@hotmail.com
Received for publication January 21, 2009 Accepted for publication April 9, 2010
SUMMARY
Introduction:
Primary esophageal myxoid liposarcoma is exceedingly rare. Sarcomas
make up 1% of esophageal malignant tumors. There are only five (5)
cases reported with this histological variant (myxoid) in previous
literature. In Colombia, this is the first case reported and the sixth
in the world.
Objective: To
report the first case in Colombia of myxoid liposarcoma of the
esophagus with clinical, radiographic images, histology, surgical and
to describe difficulties in the diagnosis.
Methodology:
We reviewed the clinical history of a 28-year old male patient. He was
admitted to Hospital Universitario del Valle in Cali, Colombia with a
clinical history of dysphagia, weight loss, and excessive salivation.
The initial
examination (esophagogram, cervical CAT scan and endoscopy)
demonstrated a mass that was reported as a fibrovascular polyp. The
finding of the pathological diagnosis was myxoid liposarcoma.
Conclusions:
The rarity of this condition recommends report of its detailed
description. The myxoid liposarcoma of the esophagus can be diagnosed
if a patient has a history of a slow-growing esophageal mass with a low
tumor density in computed tomography in combination with surgical
resection and histological examination.
Keywords: Esophageal liposarcoma; Myxoid liposarcoma; Esophageal polyp; Fibrovascular esophageal polyp.
Informe del primer caso de liposarcoma mixoide en Colombia: un tumor raro
RESUMEN
Introducción:
El liposarcoma mixoide es una neoplasia maligna del mesénquima
con una presentación muy rara en esófago. Los sarcomas
representan 1% de los tumores esofágicos malignos, y este tipo
histológico es el menos frecuente. En la actualidad, se
encuentran informes en la literatura de cinco (5) casos de esta
variante histológica en el esófago. En Colombia, es el
primer caso encontrado y el sexto (6º) a nivel mundial.
Objetivo: Presentar
el primer caso en Colombia de un liposarcoma mixoide en el
esófago, sus características clínicas,
imagenológicas, histología, manejo quirúrgico y
las dificultades en su diagnóstico.
Metodología:
Se revisó la historia clínica de un paciente masculino de
28 años que ingresa por urgencias al Hospital Universitario del
Valle en Cali, Colombia, con historia de disfagia, pérdida de
peso y sialorrea. Los estudios imagenológicos como esofagograma,
escanografía cervical y endoscopia de vías digestivas
altas son consistentes con un pólipo esofágico y el
manejo quirúrgico consistió en la resección
parcial y luego la resección completa de la lesión. El
informe histopatológico de la resección parcial
comunicó un pólipo fibrovascular y el informe de la
resección completa fue de liposarcoma mixoide. Las dificultades
diagnósticas que surgieron en este caso se relacionan con otras
encontradas en la literatura.
Conclusiones: El
liposarcoma mixoide del esófago es una entidad que presenta
dificultades en su diagnóstico debido a que la
presentación clínica no es específica. Aunque en
estos casos las biopsias iniciales pueden suponer lesiones benignas,
sólo hasta el procesamiento histológico de todo el
espécimen, es posible realizar el diagnóstico de la
entidad.
Palabras clave: Liposarcoma esofágico; Liposarcoma mixoide; Pólipo esofágico; Pólipo fibrovascular gigante.
Myxoid liposarcoma is
a malignant neoplasia of mesenchymal origin with unusual presentation
in the esophagus. Sarcomas represent 1% of malignant tumors; this being
the least frequent histological type that is of difficult clinical,
imaging, endoscopic, and histological diagnosis1. Currently, there are
reports of five cases of this histological variant in the esophagus. In
Colombia, it is the first reported case until now and the sixth
according to world literature.
CLINICAL CASE
The patient was
admitted to our hospital facilities in March 2008, because of symptoms
of progressive dysphagia, loss of weight (20 kg), and esophageal
intraluminal mass) with four months of evolution. An esophagogram was
performed, revealing a major polypoid lesion in the cervical and
thoracic esophagus extending from C7 level to the carina, which was in
endoluminal position (Figure 1). Cervical scanning shows evidence of endoluminal mass image in the lower cervical esophagus and thoracic esophagus (Figure 2).
Upper
GI endoscopy reports: Easy passage through the cricopharyngeal and
immediately beneath, a grand polypoid lesion is observed (12 cm long x
2 cm in diameter), which extends to 32 cm of the dental arch. The
endoscopy concludes with the presence of an esophageal polyp.
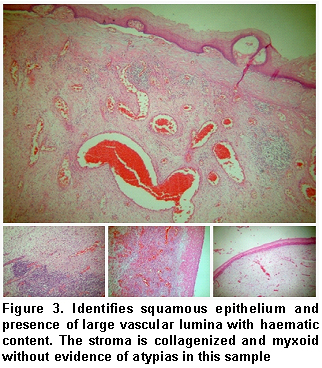
Endoscopic
partial resection of the lesion is conducted on two opportunities and
these are sent to pathological anatomy services, where the histological
findings of the two samples reveal: squamous epithelium with surface
ulceration in whose stroma there are large vascular lumina with
hemorrhagic content. There are stromal areas with mature adipose
tissue, collagenized and myxoid foci without atypia and mixed
inflammatory infiltrate. Histological conclusion yields: Giant
fibrovascular polyp1-2 (Figure 3).
The
patients was programmed for open surgery given that, endoscopically, it
was impossible to resacate the lesion. Left cervicotomy was performed
with later giant polyp removal (20 cm long); the pedicle was found in
the upper third, 7 cm from the dental arch, in addition to purulent
fluid (10 ml) and esophageal perforation (Figure 4).
Five days after the surgical procedure, the patient presents bleeding
through cervicotomy, leading to hypovolemic shock; he is intervened via
Vascular raffia procedure. Seven days after this episode, the patient
was released from the hospital -once he was able to tolerate oral
feeding. The patient was scheduled to post-surgical controls and showed
no evidence of recurrence 12 months after surgical treatment.
Macroscopically,
a specimen is obtained with polypoid aspect, measuring 20x6x5 cm,
weighing 250 grams, with ulcerated surface at the distal end. Upon
cutting, it is of myxoid aspect with adipose foci and whitish compact
nodular areas (Figure 5).
Microscopically, we
identified a malignant neoplastic lesion of mesenchymal origin,
composed of a myxoid matrix with a plexiform capillary pattern and
proliferating lipoblasts. It reveals a low mitotic index with focal
necrotic areas and hemorrhaging (Figure 6).
DISCUSSION
In the five cases
reported, until now, of myxoid liposarcoma located in the esophagus,
the patients range between 49 and 68 years of age; our case is the
first reported in a young patient (28 years of age)3-5. Regarding gender, there is a female case5 and four male cases5, predominating in males, as in our case.
Recurrence has only been reported for one female gender case5,
25 months after the polypectomy; recurrence has not been reported for
the male gender and after 12-month follow up, our patient had not
relapsed.
The first case of myxoid liposarcoma in the esophagus described in the literature refers to 19834 and the most recent refers to 19975. In Colombia, this is the first case documented and the sixth at world level, bearing in mind current bibliography reviewed.
The size of malignant neoplasias ranges between 12 and 4 cm; our case is the biggest reported with a 20 cm longitudinal diameter5.
It is common to find the histological type of myxoid liposarcoma in the
cervical site and infrequent in the distal region of the esophagus. The
transmural involvement in this histological type has not been reported
until now.
Surgery
is the treatment of choice; in these cases, polypectomy is the
procedure of choice, which was performed in the five cases reported
previously3-5 and was the procedure carried out with our patient.
CONCLUSION
The histological
diagnosis is the basis for treatment and prognosis of these patients;
given that myxoid liposarcoma is highly uncommon, frequently benign
neoplasms are considered with small biopsies.
Although
in these cases the initial biopsies may suppose benign lesions, only
after the histological processing of the whole specimen can we conclude
the diagnosis of myxoid liposarcoma.
REFERENCES
1. Minutolo V,
Rinzivillo C, Li Destri G, Scilletta B, Cammisuli F, Puleo S. Giant
esophageal polyp: a rare and benign neoplasm. Chir Ital. 1999; 51:
313-6.
2. Weiang G, Knipping L, Mangold G. Fibrovascular esophageal polyp: diagnosis and therapy. Der Chirurg. 2001; 72: 847-52.
3. Chung JJ, Kim MJ,
Kim JH, Lee JT, Yoo HS, Kim KW. Imaging findings of giant liposarcoma
of the esophagus. Yonsei Med J. 2003; 44: 715-8.
4. García M, Buitrago E, Bejarano PA, Casillas J. Large esophageal liposarcoma. Arch Pathol Lab Med. 2004; 128: 922-5.
5. Liakakos TD,
Troupis TG, Tzathas Ch, Spirou K, Nikolau I, Ladas S, et al. Primary
liposarcoma of esophagus: A case report. World J Gastroenterol. 2006;
12: 1149-52.
|