Self-rated health: Importance of use in elderly adults
José Mauricio Ocampo, MD*
* Assistant Professor, Department of Family Medicine, Universidad del Valle, Cali, Colombia.
e-mail: jmocampo2000@yahoo.com.ar
Received for publication February 19, 2010 Accepted for publication May 15, 2010
SUMMARY
Introduction: The
concept of self-rated health (SRH) was conceived during the first half
of the twentieth century. Since then, numerous studies have documented
the validity of its measurement and it has been widely accepted as a
reliable measurement of overall health. SRH is considered a subjective
measurement integrating the biological, mental, social, and functional
aspects of an individual.
Objective: To review the literature to determine theoretical determinants, related outcomes, and utility of SRH in elderly adults (EAs).
Methods:
The databases reviewed were Medline, SciELO, EMBASE, Science Direct,
Proquest, and Ovid, along with information available in websites from
international health agencies.
Results:
SRH is considered a sensitive measurement of overall health in EAs. It
is influenced by physical function, the presence of disease, the
existence of disabilities, functional limitations, and by the rate of
aging. Many studies suggest it may be modified by demographics, as well
as by social and mental factors. Thus, the perception of health is the
result of multiple and complex interactions of variables determining it
at any given time. SRH is based on systems theory and the
bio-psychosocial health model. It has proven to be a significant
independent predictor for development of morbidity, mortality, and
disability in basic physical and instrumental daily life activities
among elderly adults.
Conclusion:
In addition to reflecting the overall health status of EAs, SRH can
provide information to aid health personnel and decision makers in the
development and implementation of health promotion and disease
prevention programs, as well as the adequacy and planning of different
levels of care for this population.
Keywords: Self-rated health; Elderly adults; Daily life activities; Aging; Bio-psychosocial model.
Auto-percepción de salud: importancia de su uso en adultos mayores
RESUMEN
Introducción:
El concepto de auto-percepción de salud (APES) fue introducido a
mitad del siglo XX. Desde entonces, numerosos estudios han documentado
la validez de su medición y ha sido ampliamente aceptado como
una medida confiable del estado de salud general. La APES se considera
una medición subjetiva que integra factores biológicos,
mentales, sociales y funcionales del individuo.
Objetivo:
Realizar una revisión de la literatura para determinar
fundamentos teóricos, factores determinantes, desenlaces
relacionados y utilidad de la APES en adultos mayores (AM).
Metodología:
Se utilizaron las bases de datos Medline, SciELO, EMBASE, Science
Direct, Proquest, Ovid, así como la información
disponible en sitios web de organismos sanitarios internacionales.
Resultados:
La APES se considera una medida sensible del estado general de salud en
los AM. Está influida por la función física, la
presencia de enfermedades, la existencia de discapacidades, de
limitaciones funcionales y por el tipo de envejecimiento. Muchas
investigaciones sugieren que la pueden modificar variables
demográficas, sociales y mentales. De esta manera, la APES es la
resultante de múltiples y complejas interacciones de variables
que la determinan en un momento dado. La APES se fundamenta en la
teoría de sistemas y en el modelo bio-psicosocial de salud. Se
ha demostrado que se comporta como un predictor independiente y
significativo para desarrollar morbilidad, mortalidad y discapacidad,
tanto en las actividades básicas cotidianas como en los aspectos
físico e instrumental en adultos mayores.
Conclusión:
La APES además de reflejar el estado de salud global del AM,
puede brindar información que ayude al personal de salud y a
tomadores de decisiones en el desarrollo e implementación de
programas de promoción de la salud y prevención de la
enfermedad, así como en la adecuación y
planificación de diferentes niveles asistenciales para este
grupo poblacional.
Palabras clave: Autopercepción de salud; Adulto mayor; Actividades básicas cotidianas; Envejecimiento;
Modelo bio-psicosocial.
Population aging is
probably the most important demographic phenomenon in the world during
the end of the 20th century and beginning of the 21st century1.
The population of elderly adults (EA), defined as individuals 60 years
of age and older present 2.4% growth rates, compared to 1.7% for the
total population. It is expected that this growth rate increases by
3.1% as of 2010. In absolute numbers, this shows that the EA group will
increase from 616-million in 2000 to 1.209-billion in 2025, implying
that this population group will double in numbers every 25 years1.
The
aging process can lead to gradual deterioration of mental and physical
health conditions, reduction in expected years of active and healthy
life, and complete or partial cease in participation in the labor market2.
Likewise, alterations in the health status -characteristic of advanced
age- are more chronic than acute and more progressive than regressive.
This makes it necessary to know the state of health of this population
so it can be intervened from the vantage point of health promotion and
disease prevention, as well as for the adequacy and planning of the
care offered and for the development of health programs.
To
accomplish this, it is necessary to start by being clear on the concept
of health status as defined by the World Health Organization (WHO) in
1945, thus: «A complete state of physical, mental, and social
wellbeing and not merely the lack of disease or disability»3.
This definition, in schematic manner, circumscribes health within a
quadrant in which the extremes correspond to the physical, mental,
social, and spiritual dimensions. Additionally, it is stressed that the
concept of health should bear in mind the human being as a total and
integral being. This focus permits visualizing the four dimensions
mentioned in independent and integrated manner in individuals, in whom
these dimensions function as a complete entity and in relation to the
world around them.
Consequently,
this holistic view makes the assessment of the state of health to
become a complex activity, particularly in EAs because during the aging
process a series of internal and external modifications take place, as
well as changes in the functions of the individual’s organs and
systems. This becomes evident when the person is exposed to stressful
situations that induce changes in the state of health, as a product of
lower functional reserve and lower capacity for response and
adaptation, a phenomenon known as homeoestenosis, which can lead to
greater probability of organic failure and illness4.
With
respect to assessment of state of health in EAs, it is fundamental to
bear in mind that it is integral and such then go beyond the
traditional clinical history. Therefore, this assessment must consider
the psychological, familial, social, economic, and functional dimensions5.
It is worth mentioning that this assessment, more than in other age
groups, implies subjectivity, because it depends on the interaction
among physiological conditions, functional abilities, psychological
wellbeing, and social support. For this reason, the evaluation of the
state of health should not bear in mind only the strictly medical
aspects, it should go beyond, being relevant for clinicians, decision
makers, and researchers working with this population group5.
WHAT IS SELF-RATED HEALTH STATUS AND WHAT ARE ITS ORIGINS?
In spite of the
generalized use of the term self-perception, there is no clear
definition of its meaning in scientific literature; there is also no
clarity of its theoretical concept. Self-perception can be defined as
the concept individuals have of themselves and based on such; they
process and organize the information of their context within a
structure that provides the basis of principles to act in the present
and in the future. Thus, individuals maintain and develop a basic
scheme of their own self-perception throughout their whole lives6.
Self-Rated
Health has been employed in a broad variety of scenarios with different
population groups and for a great number of objectives ranging from
screening for specific health conditions to studies designed to aid in
decision making for individuals in crisis situation, like depressive
states or the capacity to decide on changing domicile7. As
mentioned, in the previous paragraph the term SRH has been used to
refer to the response made by individuals when asked about their state
of health; hence, it can be applied to all self-reports of state of
health or of specific symptoms like pain or the sensation of dyspnea,
fatigue, or tiredness7.
In
other words, SRH is a way of evaluating the state of health in people,
which integrates information on the biological, mental, functional, and
spiritual dimensions of an individual’s health8.
Thereby, it is considered that SRH represents the perception
individuals have of the different dimensions of their state of health;
accordingly, SRH can be classified as a result and integral variable,
which permits inferring that it can encompass the different dimensions
of the human being9.
The SRH
concept has been included in different research projects since the
1950s and ever since then diverse studies have shown its usefulness in
documenting the state of health self-reported by EAs during a given
moment and also in predicting future health-related events8,9.
This shows the great interest in using SRH when conducting research
that assesses state of health; in fact, it is already part of health
surveys carried out with EAs.
WHAT ARE THE THEORETICAL FOUNDATIONS OF SRH?
For the theoretical
understanding of SRH, a model made up of four dimensions is proposed.
Said dimensions are defined by their content, i.e., by the aspect each
seeks to evaluate. In turn, between dimension and dimension there are
multiple interactions. The type of self-perception we wish to assess
depends on the dimension predominating in such interaction and on its
characteristics, for example, if the approach tends to be more general
or specific and if it seeks to evaluate social aspects, health aspects,
or both7 (Graphic 1).
Hereinafter,
we present the different approaches of the evaluation according to the
dimensions and type of self-perception, based on the proposal by
Griffiths et al.7
·Health care approach. This
domain focuses on assessing specific health aspects and problems.
Self-perception can collaborate and, on occasion substitute the
assessment made by the health professional. For example, based on this
domain, research has been conducted to identify elderly adults with
mental disorder, hearing and vision loss, and problems with nutrition,
mobility, and function. This type of self-evaluation can help to
predict current needs and some future ones. When an approach to
self-perception is conducted through this domain, the
individual’s internal factors are exclusively considered.
· General health care approach.
This domain is used for evaluating a broad range of factors related to
health care. The objective here is to improve general health care and
mediate in the patient’s relationship with healthcare
professionals. Mental health status, functional capacity, social
contacts, and use of health services are among the aspects investigated
in this domain. This type of assessment permits determining the
individual’s current needs, and can sometimes aid in predicting
future needs, although it does not permit identifying the resources
available for the individual. When approaching self-perception through
this domain, internal and external factors of the individual are
considered.
· Social care and abilities for life approach.
This domain focuses on assessing everyday situations and aspects the
health professional does not frequently evaluate during consultation,
like the individual’s capacity to drive a vehicle and the
possibility of being involved in accidents. Aspects related to home
safety along with risks of falling are also assessed. This provides
greater elements for patient assessment and care. When approaching
self-perception through this domain, internal factors of the individual
are considered, as well as external factors like environment,
employment, and leisure time.
· Multidimensional approach. This
domain involves external factors like social aspects and internal
factors like the individual’s state of health and wellbeing. The
main objective of this domain lies in identifying necessities and
offering information that permits the individual to adequately satisfy
such. Because of the great number of factors this domain can encompass,
it is possible that it includes elements of self-assessment of social
care along with life skills and the impact of the state of health. The
distinction between the domain of general health care and the
multidimensional approach lies on the balance and weight given to
health problems and services. If the approach is multidimensional, a
global approximation is made of the aspects related to the
individual’s state of health, unlike general health care that
emphasizes health needs and services for the individual.
Different
research has shown that measuring personal health perception is a
useful global indicator of the population’s level of health,
given that it reflects social and biological elements10,11.
In effect, SRH is one of the mostly used types of self-perception to
determine the state of health in EAs from a subjective perspective,
because it shows multiple aspects of the individual’s state of
health that could turn out to be difficult to obtain via traditional
quantitative research methods. For example, objective measurements
often evaluate only one aspect, as with levels of glycated hemoglobin
that are used in determining the state of control of diabetes mellitus.
It could be said that the subjective and objective measurements are
complementary and necessary when learning of the individual’s
state of health. Consequently, SRH is considered a type of
self-perception employing elements from the multidimensional approach
according to WHO recommendations12.
For the theoretical explanation of SRH, we used the bio-psychosocial model suggested by Engel13,
which approaches health from a holistic view and which considers the
individual a being participating in the social, psychological, and
biological spheres; in contrast to the analytical, reductionist, and
specialized biomedical model, which additionally takes into account the
person as an object and ignores that person’s subjective
experience as a possibility of also being studied in scientific manner14.
On the
contrary, the bio-psychosocial model considers an illness not as the
lack of health or simply physical health but also any psychological or
social interaction that can affect and individual’s state of
illness/disability.
Understanding
the bio-psychosocial model requires an approach to the General Systems
Theory, whose main exponent was Ludwig von Bertalanffy15,
and stemming from this approach there can be integration between the
parts and the whole, where relationships are not unidirectional but
bidirectional and there is no cause and effect unicausal relationship,
but one of multifactorial effect. With this, an important change is
produced given that understanding the phenomena the simple thought
«first A then B» is not sufficient, but rather the capacity
of thinking of the complexity of the multiple interactions.
With
respect to the SRH model suggested, a set of independent variables is
shown that are grouped according to the state-of-health dimension to
which they belong in social, demographic, biological, mental, and
functional terms. From a subjective perspective, individuals will
self-report their state of health. This implies that people must
undergo complex reasoning involving multiple interactions of
independent variables for the self-report of the state of health.
This
interaction of multiple variables permits obtaining information on the
state of health of the elderly adult during different moments, i.e.,
the current state of health compared to that of other individuals of
similar age and the current state of health actual compared to that of
the previous year. Additionally, said interaction may offer prospective
elements that help to anticipate the development of any given event in
the future.
On this
matter, SRH behaves as an intermediate variable among the independent
variables that determine it and the different outcomes to which it has
been associated like death, hospitalization, and functional impairment
among others16 (Graphic 2).
WHY IS THERE INTEREST IN RESEARCHING SRH?
Many health
professionals treating elderly adults focus mainly on factors related
to physiological measurements (laboratory values), mental state
(presence of depression), life styles (smoking habit), or functional
state (Basic Daily Activities). However, studies have shown that the
perceptions offered by EA son their state of health and wellbeing can
be as important as the clinical variables to evaluate and predict the
evolution of the state of health over time9.
Unfortunately,
current clinical medicine practice has progressively stopped listening
to patients (their ailments), and has replaced this for observation or
measurements like diagnostic images or application of scales17.
This has caused medicine to go from being a discipline involved with
listening and feeling, to a discipline of seeing and doing; proof of
this is the increase in the algorithms and guides for clinical practice
in recent years. That could explain why the question on the perception
of the state of health is often ignored; in fact, the medical practice
prefers to inquire more about quantitative than qualitative aspects,
for example, on inquiring about sleep the question is how many hours
does the patient sleep per day, rather than how does the patient feel
with his/her sleeping habits18.
As has
been insisted upon in this article, different studies have shown that
assessing the personal perception of the state of health is useful
because it allows globally describing the population’s level of
health given that it reflects elements that are not merely biological,
but also psychological, social, and functional10,11. It has
also been employed to compare the state of health of EAs from different
countries, because it can be easily obtained and reflects multiple
aspects of the state of health that could be difficult to gather by
other methods19.
Analyzing
the factors related with SRH will permit identifying health needs and
evaluating programs and interventions aimed at EA population group.
Hence, it should be included in research for the following reasons9:
·
It is a global measurement of the state of health, psychological
wellbeing, and quality of life related to health, offering much more
information than other variables used in traditional research, for
example, the presence of chronic illness or total cholesterol values,
among others.
· It is easily
obtained through one single question: «Do you consider your
general health status: excellent, very good, good, regular, or
poor?» This shows that specialized personnel are not required to
assess a population’s general state of health.
· It is an
indicator significantly associated with the population’s state of
health and with mortality; consequently, it can be used approximately
to determine healthcare needs.
· It behaves as
a screening test because it helps to identify high-risk individuals in
prodromal stages for the development of adverse health events like
falls, and hospitalization among others.
· At the
individual level, it may predict mortality in the elderly; thereby,
useful in current or future behavioral models to determine, for
example, the use of retirement services or plans.
·It may be used to tailor health services and establish priorities in healthcare.
WHAT STUDIES HAVE BEEN CONDUCTED IN LATIN AMERICA ON SRH IN ELDERLY ADULTS?
In Colombia, not much research has been done on SRH in EA populations. One of these was done by Gómez et al.20
who carried out an observational analytical, cross-section study in the
city of Manizales, where SRH assessment was done and established a
correlation with the presence of co-morbidity and functional state. The
researchers found an important association among SRH, chronic disabling
disease, and functional capacity, measured via the Barthel scale, which
evaluates Basic Daily Activities in the physical aspect.
Recently, Parra et al.21
conducted a multilevel observational analytical, cross-section study to
determine the association between urban and environmental
characteristics in the city of Bogotá with SRH and quality of
life related to health. A positive association was found between
perception of neighborhood safety with good SRH and quality of life
related to health. Likewise, the availability of recreational spaces
like safe parks that promote social interaction and recreational
activities was associated to good SRH and quality of life in the mental
health domain. On the contrary, zones with high levels of noise were
associated to bad SRH and quality of life. The value of this research
lies in that it is the first study conducted in a highly urbanized city
in a country with low to medium economic income. Additionally, it
offers inputs to implement interventions aimed at improving the quality
of life and SRH of EAs living in cities with environmental and
socioeconomic characteristics that are similar in several Latin
American nations.
Hambleton et al.22
carried out an observational analytical, cross-section study, employing
information belonging to the population of Barbados in the «SABE
project», which is a multicenter survey conducted in seven urban
centers in Latin America and the Caribbean to evaluate the factors
impacting the health and wellbeing of EAs 60 years of age or more. The
study sought to determine the relative contribution of past events and
current experiences to the state of health of EAs for the purpose of
conducting opportune sanitary interventions for said population. It was
found that past experiences of socioeconomic aspects influenced SRH,
and over half of the influence exerted by past events was measured by
current experiences related to the socioeconomic situation, life style,
and the presence of illnesses. Therefore, when caring for the elderly,
consideration must be made for intervention of the risk factors related
to life style. The importance of this research lies on the relationship
established by the authors between social and clinical determinants
with SRH. Consequently, when implementing programs to reduce poverty
and increase Access to healthcare and education, long-term strategies
should be considered aimed at improving the health of the elderly of
the future.
Alves et al.23
employed information from a population in Sao Paulo, Brazil from the
«SABE project» to carry out an observational analytical
cross-section study. The purpose of that work was to determine, via
SRH, the relationship between demographic, social, and economic factors
along with the presence of chronic disease and functional capacity in
EAs 60 years of age and older. The study also sought to evaluate if
there were gender differences. It was found that presence of chronic
disease in relation to gender was the greatest association to determine
SRH, i.e., males presenting four or more chronic illnesses had 10.53
times greater opportunity for bad SRH; similarly, for females it was
8.31 times. Likewise for educational level, income, and functional
capacity were related to SRH. The novel aspect of this research is the
approach of SRH from the multidimensional perspective, and that it may
be useful for decision makers when implementing actions from the health
sector seeking to promote wellbeing and quality of life for the elderly.
Reyes et al.24 led
an observational analytical cross-section study, employing information
from the multicenter survey in the «SABE project». The aim
was to determine the relationship between religiosity and SRH. It was
found that most (90%) reported having some religious affiliation, and
within this group 80% considered religion important in their lives. The
EAs who considered religion very important in their lives had lesser
opportunity of reporting bad SRH when compared to those who considered
religion less important. This is one of the first studies carried out
in urban centers in Latin America and the Caribbean showing the
importance of religiosity in the state of health of elderly adults.
HOW IS SRH MEASURED?
In recent years,
surveys employed to assess state of health have used diverse questions
trying to integrate the different dimensions of the human being25.
These types of surveys take into account the self-report of health,
through a subjective, global, and integrating evaluation of the state
of health done by the individual. This includes the perception of small
physiological-type variations, negative or positive attitudes on life
and disposition for healthy conducts; these are related to clinical
morbidity, which is influenced by social, cultural and emotional aspects7.
To
assess SRH, a variety of schemes of structured questions has been
designed with their possible responses, among which there is the WHO
version employed in Europe and the United States version.
The
World Health Organization version, which is recommended and used in
Europe, takes a range of responses from very good to very poor. It is
characterized because it groups the responses into several categories,
of which two are positive (very good and good); one neutral (regular);
and two negative (poor and very poor)12.
The better known United States version is employed by Bjorner et al.26
who initially used the question: How do you rate your state of health?;
with four possible response options: excellent, good, regular, or poor.
Then, a fifth «very good» response option was added, along
with an additional question on the current general state of health
compared to that of the previous year: How would you rate your current
general state of health, compared to that of the previous year? which
is how it is known and applied currently in different research
projects. These last additions were included because of the study
conducted by Ware et al.27 who used the abbreviated SF-36 form.
Regarding
SF-36, this is the instrument developed for use in the Medical Outcomes
Study, from an extensive battery of questionnaires, whose final format
provides a profile of the state of health28. It includes 36
points grouped into 8 scales: physical functioning, physical
performance, body pain, emotional performance, mental health, vitality,
general health, and social functioning, plus an additional one: change
of health over time. These points assess positive and negative states
of mental and physical health. For each dimension, the points are
coded, aggregated, and transformed into an ordinal scale ranging from 0
(the worst state of health for that dimension) to 100 (the best state
of health), without generating a global index.
This
instrument has been used in over 40 countries in the International
Quality of Life Assessment Project. It is documented in more than 1,000
publications; its usefulness in estimating disease burden is described
in over 130 conditions and it is used worldwide because of its
briefness and comprehension. It is worth pointing out that in the
assessment made on Colombian adults a Spanish version was obtained
showing complete coincidence with the expected original, high
equivalency with the original values, and acceptable reproducibility,
concluding that the SF-36 is reliable in evaluating healthy quality of
life after it was linguistically adapted in Colombian adults29.
After
evaluating self-perception with a single question, SRH was used to
assess the perception individuals have of their own health in
comparison to other people of the same age; this provides greater
information than that offered by the concept of personal self-perception26. Table 1 shows the different questions that can be made when assessing state of health via SRH.
Also,
when comparing the two questions with their possible responses to
assess SRH, it has been found the WHO version discriminates the
negative categories better, unlike the version from the United States
that discriminates the positive categories better30.
However, both types of questions are highly correlated and have shown
similar associations with respect to demographic variables and health
conditions, as well as having a similar variation pattern when applied
in different countries31.
WHAT FACTORS DETERMINE SRH?
Self-rated Health may
be considered a global result of the measurement of multiple factors
determining it. In fact, it is influenced by demographic variables like
gender and age; social variables like social networks and family
functioning; biological variables like the presence of illnesses and
taking of medications; mental variables like suffering anxiety,
depression, dementia, or grief; and, lastly, functional variables like
presenting commitment in the physical and instrumental Daily Basic
Activities8.
The different factors determining SRH by group of variables are:
Demographic variables.
Regarding differences in SRH according to gender, diverse explanations
have been considered among which there are differences in the state of
health, wellbeing, and functionality and not in the greater or lesser
possibility of one or the other sex reporting a determined state of
health. This means the relationship between SRH and gender is mediated
by other factors like educational level, illnesses, depression, and
functional state. Here, it is worth mentioning that women report a
greater proportion of health problems and have greater diagnosis of
diseases like arterial hypertension, diabetes, musculoskeletal
disorders, and accidents, aside from presenting greater frequency of
affective disorders when compared to men. Given that women have higher
life expectancies and, therefore, a greater possibility of enduring
chronic disease that deteriorate their functionality, as those already
mentioned, this could explain why they evidence greater association
with the self-report of a bad SRH32.
Adding
to the aforementioned, women have a higher life expectancy than men.
This occurs at the expense of years lived with greater functional
deterioration, that is, the consequences of the disease affect the
internal and external perception of reality and translate to diminished
quality of life when diminishing the possibilities of being and doing,
which leads women to deteriorated perception of their own health and
limitation of activities, functions, and opportunities11. Thus, better SRH has been constantly found in men than in women and this is more notorious in the elderly.
Another
factor to bear in mind and that may explain a greater frequency of bad
SRH in women is their lower income, which diminishes as they get older,
and especially when they are very old10.
It has
also been postulated that with the passage of time in the elderly, SRH
tends to regular or poor, which can be explained by multiple factors,
including the loss of social roles, chronic disease and disability
among others20. In spite of this, individuals over 90 years of age may
paradoxically manifest good or excellent SRH, explained by different
factors among which include:
·
Heterogeneity of the aging process, which postulates that over the
years – in spite of higher risk of illness and deterioration of
the functional state, the elderly do not necessarily uniformly or
inevitably manifest bad SRH18.
· Elderly
adults take as reference groups other older individuals in whom
disabilities are the norm, which leads them t orate their health
positively; additionally, over time they start establishing adaptive
mechanisms to accept their own aging process, the presence of chronic
disease, and functional limitations33.
· Elderly
individuals are more optimistic regarding their health as they age,
because they have become accustomed and perceive illnesses and
functional impairment more optimistically than the younger individuals34.
· The survival
effect, i.e., those reaching 85 years of age constitute the group with
the highest optimism; while the most pessimist regarding their health
may have already perished35.
· Elderly
adults are a group that along the years has been exposed to multiple
stressing events and subject to natural selection so survivors tend to
be stronger and healthier34.
In
addition, with the passage of years SRH may have multiple paths, which
are determined by diverse bio-psychosocial factors, consequently
presenting great variability among individuals, which could also be
related with the type of aging shown by the EA. The types of aging that
have been described are successful, usual, or pathological36.
EAs with successful aging, unlike those with usual or pathological
aging, show high levels of physical, mental, and cognitive functioning,
as well as lack of or low probability of developing disease or
disability and an active commitment with life. EAs with usual aging
present non-pathological losses related with age and in pathological
aging there is evidence of disease with disability and its multiple
bio-psychosocial consequences36.
Regarding
the relationship between the type of aging and SRH, it has been
suggested that EAs with successful aging show good and stable SRH over
time; however, SRH begins to deteriorate after 80 years of age.
Nevertheless, paradoxically in some EAs 85 years of age and above SRH
can stabilize or improve, which is explained, as mentioned before,
because it is an optimistic group and because it is the result of
natural selection37. The elderly with usual aging report SRH
similar to EAs with successful aging although the SRH impairment
process begins earlier, around 70 years of age. Finally, EAs with
pathological aging have bad SRH as a base and their impairment
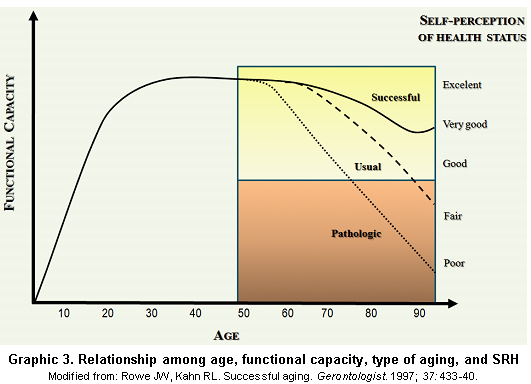
accelerates after 60 years of age34. Graphic 3 displays the relationship among age, functional capacity, type of aging, and SRH.
A
strong association has also been found between SRH and the
population’s socioeconomic level, given that the general state of
health is better in individuals with higher socioeconomic levels11.
However, exceptions are possible, particularly in certain populations
of elderly adults, because this is a very heterogeneous group and this
aspect may lead to important differences in the self-report of health19,37.
Educational
level is considered an important aspect determining better or worse
SRH, inasmuch as individuals tend to have a better perception of their
health when they have higher educational levels although they may have
a greater number of illnesses26. It is considered that
according to the educational level, the individual may have better
tools to face vital stressing moments and, consequently, may modulate
the result of SRH14.
Regarding
geographical location factors influencing SRH assessment, it has been
found that these differ from one country to another38. This
diversity of patterns may be due to the demographic and epidemiological
transition stage in which the populations are found39. For
example, in healthier populations the perception of better health may
depend to a greater extent on emotional health, on chronic disease, or
on functionality problems; while in populations with the worse health,
the general self-evaluation of health may be more affected by other
health problems like infectious disease38. Another possible
explanation for the differences found is that individuals with similar
levels of health perceive their state of health differently in
relationship with determined structural elements of the national
sanitary systems like quality of healthcare services or the importance
given to the illnesses they suffer19.
Likewise,
the use of healthcare services may be associated with the evaluation of
SRH; lowered use of sanitary services indicates better self-perception26.
Results of longitudinal studies have revealed that survival is more
related with subjective than with objective health and that healthcare
is one of the factors associated with satisfactory aging35.
Although
the subjectivity of SRH is acknowledged because it accounts for the
perception people have of their own health, this may have advantages in
cases where the population does not have generalized access to
healthcare services37. Much of the information about the use
of SRH in elderly adults and its relationship with other indicators
comes from developed nations8. The assessment of the
usefulness of this indicator in developing nations recently emerged
with studies carried out in some countries in Latin America and Asia38.
In
developed nations where there is greater contact between the population
and sanitary personnel, it is possible that the self-report of specific
disease like diabetes, arterial hypertension, or cancer is a better
indicator of the population’s health, because it is more
objective than the general evaluation of one’s own health40. However, even in developed nations, the self-report of specific disease may enclose large bias41.
In
general, it is suggested that during old age the decline of the ego is
intensified, deriving into a loss of identity, low self-esteem, and
decrease of social conducts2. In spite of the
aforementioned, having a stable relationship like a matrimony,
participation in community activities, and joining social groups may
help to maintain a sense of continuity including a more positive SRH,
even after retirement37.
Biological variables. Prior
awareness of an illness, particularly of chronic disease, suffered by
the person, may affect the judgment the individual has of SRH42.
Self-Rated
Health is specially influenced by somatic experience that generates the
illness. Somatic experiences are physical manifestations that may be
represented, for examples, by fatigue or a sensation of dyspnea, which
can make individuals interpret they are suffering a serious condition
and, consequently, modify their SRH. Knowledge of a potentially life
threatening, serious disease like coronary disease or cancer, may have
a greater impact on the individual, unlike knowing of a disease that
impairs functionality but is not life threatening like osteoarthritis
or hypertension, may lead to modifications of activities or behaviors
and especially a change in SRH. Hence, SRH is considered the product of
a process depending to a great extent on the information the individual
has of the subjective experience generated by the disease43.
The
presence of a disease may modify SRH, as can the clinical course; some
diseases, especially those involving organic systems, like congestive
heart failure, have periods of clinical stability but can also be
intercalated with periods of exacerbation. Thus, SRH represents a
complex judgment made by the individual at a given moment on the
severity of the current state of health, because the course of a
disease can be modified over time.
Also,
in spite these being personal perceptions EAs of their own health, some
studies have shown that the morbidity they perceive coincides by two
thirds with that diagnosed by health professionals32. In
studies, it has often been found an excellent or very good SRH in
individuals with good physical health; however, paradoxically, it has
also been noted that individuals with these same physical health
characteristics have regular or poor SRH. Later analyses have shown
that these individuals have symptoms of depression or dissatisfaction
with their lives18.
Mental variables. One
of the reasons why the self-concept, SRH, and their relationship with
age suppose a problem is the perception by EAs of feeling
psycholo-gically worse34. Indeed, depression is one of the
most frequent mental disorders for EAs. Prevalence for major depression
has been described at 1%-5% and a frequency of 8%-27% for significant
symptoms of depression in EAs living in the community44. The prevalence is greater in hospitalized elderly subjects, and in those living nursing homes45.
Frequently, depression emerges in EAs in atypical manner and does not
fulfill the clinical criteria for major depression. These incomplete
syndromes are denominated minor depression or subsyndromal depression
according to the diagnostic statistical manual for mental disorders
(DSM-IV) and have the same repercussions, in terms of morbidity and
mortality, as major depression46.
Depression
may involve cognitive processing, causing individuals to manifest lower
satisfaction with their lives and, consequently, worse SRH. Studies
have shown that EAs with depression or dementia reveal worse SRH
compared to those who do not present any of these disorders9.
The
evaluation of SRH in EAs with depression, dementia, or delirium may be
complex. Cognitive impairment, per se, acts as an independent
predictor for mortality47.
Regarding
the relationship between the cognitive state and SRH, some authors
consider that cognitive alteration may make the SRH report unreliable,
particularly in patients with dementia48.
Others, on the contrary, consider that SRH is not altered. Walker et al.49
conducted a prospective population study with 8,697 elderly adults
living in the community in ten Canadian provinces to evaluate if SRH
behaved as an independent predictor for survival and determine if the
cognitive function could modify such relationship. It was found that
SRH was a valid measurement and predictive of survival in elderly
adults with minimal, slight, and moderate cognitive impairment. This
shows the complexity of the cognitive process in said relationship and
given that SRH is a subjective measurement it may reflect the state of
health the same way other objective measurements do, like the presence
of co-morbidity or the assessment of the functional state, within a
broad range of cognitive functioning.
Functional variables.
It is suggested that many chronic diseases have direct effects on SRH,
independently of the presence of disability or functional limitation.
Lammi et al.50 concluded that in contrast to the Framingham
study, diseases by themselves are stronger predictors of disabilities
than unhealthy habits, and that EAs judge their quality of life and
their health, more from the point of view of the capacity to
independently perform or not their daily life activities.
Likewise,
there is awareness of the association between co-morbidity and
functional impairment in physical and instrumental Basic Daily
Activities. Indeed, and as was already mentioned throughout this text,
the functional state is an important factor in determining SRH, which
shows the complexity of the multiple interactions existing between the
different factors determining it51.
From
another vantage point, although functional impairment and the presence
of chronic disease are important factors for the formation of the
subjective concept of a bad SRH; in spite of this, EAs with chronic
disease may report a good SRH. Such is the case of the Ontario health
survey conducted in 1990, where it was found that 79% of those with
chronic disease and 50% of those with long-term disability reported
good or excellent SRH52. This suggests that in spite of the
presence of chronic disease or disability, many EAs can perceive their
state of health favorably.
WHAT ADVERSE HEALTH EVENTS CAN SRH PREDICT?
Self-Rated Health has
been associated with health events like disease, death,
hospitalization, and functional impairment among others; however, some
of the factors determining SRH have also been associated independently
to health events, which lead to inferring that SRH acts as an
intermediate variable.
The
capacity of SRH to foresee morbidity has been considered good. Some
studies have shown that perceived morbidity coincides by two thirds
with morbidity diagnosed by healthcare personnel32. The
variables with greater association with the self-report of poor SRH are
the presence of chronic disease like hypertension, diabetes, urinary
tract disease, renal failure, acute illness, and functional like being
disabled, suffering a mental or physical disability or limitation53.
Hence, the perception of health and the factors associated with such
may be used to assess the level of health of the population of elderly
adults and its determinants53.
Also,
during the last 20 years there has been an important increase in
studying SRH as a predictor of mortality. Most studies find a
significant association between SRH and mortality54. Others
have found that the predictive value decreases, even losing its
significance when the analysis is adjusted according to other factors,
like prior morbidity or functional capacity55. Differences
in adjustment variables are also mentioned in the perception due to
gender or idiosyncratic variations in the population studied16.
Among
the arguments postulated to explain the capacity of SRH to predict
mortality, we have found, in the first place, past and current
knowledge of the health experience implying that EAs make a comparison
of their own health with people of similar age and state of health, and
in the second place, the personal health practices influencing on the
health results56.
The
relationship among SRH, mortality, and gender, is controversial. In
some studies, a stronger association has been demonstrated in males
than in females and a loss of meaning has been observed in women when
adding other variables, like the objective state of health when
participating in the interview57. In contrast, other studies have found the opposite effect, with a stronger association in women58.
These differences among different studies may be explained by the fact
that SRH does not have a unique point of reference; individuals use
personal perceptions, information from their neighbors and friends, as
well as objective medical information to have an idea of their state of
health.
Also,
regarding the relationship among socio-demographic factors, SRH, and
mortality, it is considered that said information may differ according
to gender, the moment of the vital cycle, or the social context. For
these reasons, it is interesting to study the relationship between SRH
and mortality in different populations and with different social
contexts59. The results among these three aspects,
socio-demographic factors, SRH, and mortality, have been contradictory
because some researchers have found that poor SRH is associated to
increased risk of death, even after adjusting it according to a broad
spectrum of socio-demographic variables acting as potential confounders16.
Other studies have not found a clear relationship between SRH and
mortality after adjusting it according to demographic, socioeconomic,
and clinical variables or psychosocial factors9. Some
authors have suggested possible explanations for these contradictions,
which include differences in the methods and ways of making the
questions and different types of response forms. There is also
reference to differences in the variables used for adjustment,
differences in perception due to gender or variations in the
idiosyncrasy of the population studied16.
It is
worth pointing out that studies in which the relationship between SRH
and mortality has been researched, the question has been dichotomized
in the following manner: good with options good and excellent and poor,
which includes regular, poor, and very poor. Furthermore, by including
multivariate logistic regression models, it was possible to evaluate
the association between SRH and mortality by adjusting for different
variables like chronic disease, habits (smoking, alcohol),
functionality, socioeconomic level, and others. When introducing these
analysis models, from decreased relative risk to a slight increase in
the association have been found. For example, a study carried out with
elderly Finish men during a 6-year period revealed a decrease in the
association of relative risk between mortality and poor SRH, which
decreased from 3.76 to 2.12 when the analysis was adjusted for eight
risk factors (body mass index, smoking, HDL cholesterol, LDL
cholesterol, blood pressure, physical activity, alcohol consumption,
and income)60. When a further analysis was done for eight
chronic diseases, the association diminished to 1.69. There is a
quantitative-type interaction because the means of association of the
effect have the same direction. Additionally, although the last
relative risk is lower, it is statistically significant and represents
a 69% increase in mortality for individuals reporting poor SRH.
Regarding
the relationship among measurements of SRH repeated over time and its
capacity to predict adverse health events, mixed results may be found.
Leinonen et al.61 conducted a cohort study with elderly
Finish subjects and after a follow up of the subjective assessment of
the state of health, they stated that stability is more common than
change in this assessment and systematically reflects the health
conditions, the functional capacity, as well as physical and social
activities. For the authors, the high stability in self-perception
indicates that with increased age, the elderly subjects adapt to worse
health conditions. This adaptation plays an important role that is
reflected in the subjective evaluation. Thus, the evident deterioration
in the objective evaluations is not subjectively reflected and the
authors suggest that the adaptation strategies to this deterioration
are given by modifications of expectations, aspirations, and standards
or that they see it as part of the normal aging process and adjust
their standards of good health accordingly. Furthermore, age-related
impairment is usually a gradual process to which they adapt slowly,
without simultaneously modifying their SRH; that is, there is a
cognitive reorganization for new internal processes. The stability may
also indicate comparison with other individuals in worse conditions or
with greater disadvantages. The few fluctuations in self-perception are
given by big or abrupt changes in the state of health or in the
symptomatology of the diseases, which also cause changes in the
functional capacity61. Given that SRH depends upon multiple
factors and among these there are the socioeconomic variables, said
hypotheses should be proven in developing nations so they can be
accepted and in this sense avail of their usefulness in our environment38.
In
terms of the cognitive function and the relationship between SRH and
mortality, it is known that SRH may adequately predict mortality in EAs
with slight, minimal and moderate cognitive impairment. For severe
impairment, its capacity to predict is affected and factors like age
and functional impairment take on greater importance49.
Likewise,
SRH has been associated as a predictive variable for hospitalization,
development of falls, functional impairment in the physical and
instrumental Daily Basic Activities, a greater demand for healthcare
services and institutionalization in nursing homes, after being
adjusted for possible confounding factors like socio-demographic
variables16.
In
conclusion, the concept of SRH has been broadly used, given that it is
a reliable and easily obtained measurement of the general state of
health, because it permits integrating a subjective measurement as an
indicator. Self-Rated Health is determined by the physical function,
the presence of disease, the existence of disabilities and functional
limitations. It has been associated with adverse health events like
mortality, use of healthcare services and impairment of physical and
instrumental Daily Basic Activities, becoming an important variable to
assess the state of health in the elderly.
REFERENCES
1. Manton KG,Gu X, Lamb VL.
Change in chronic disability from 1982 to 2004/2005 as measured by
long-term changes in function and health in the U.S. elderly
population. Proc Natl Acad Sci. 2006; 103: 18374-79.
2. Ocampo JM, Londoño I. Ciclo vital individual: vejez. Rev Asoc Colomb Gerontol Geriatr. 2007; 21: 1072-84.
3. WHO. Constitución de la Organización Mundial de la Health- Geneva, 1945. Date available: 6 November 2009.
4. Ocampo JM. Estrés y
enfermedades del adulto mayor. En: Herrera JA (ed).
Psiconeuroinmunología para la práctica clínica.
Cali: Programa Editorial Universidad del Valle; 2009. p. 109-28.
5. Ocampo JM. Evaluación geriátrica multidimensional del anciano en cuidados paliativos. P & B 2005; 9: 45-58.
6. Meléndez JC. La autopercepción negativa y su desarrollo con la edad. Geriatrika. 1996; 12: 389-1996.
7. Griffiths P, Ullman R,
Harris R. Self-assessment of health and social care needs by older
people: a multi-method systematic review of practices, accuracy,
effectiveness and experience. London: NCCSDO, 2005. Date available: 18
December 2006. Available in: http://www.sdo.lshtm.ac.uk/sdo302002.html
8. Bjorner, JB, Kristensen
TS, Orth-Gomér K, Tibblin G, Sullivan M, Westerholm P. 1996.
Self-rated health: A useful concept in research, prevention and
clinical medicine. Stockholm: Swedish Council for Planning and
Coordination of Research.
9. Idler EL, Benyamini Y.
Self-rated health and mortality: a review of twenty-seven community
studies. J Health Soc Behav. 1997; 38: 21-37.
10. Aspiazu GM, Cruz JA,
Villagrasa FJR, Abanades HJC, García MN, Valero FA. Factores
asociados a mal state of health percibido o mala calidad de vida en
personas mayores de 65 años. Rev Esp Health Publica. 2002; 76:
683-99.
11. Damian J, Ruigomez A,
Pastor V, Martín-Moreno JM. Determinants of self assessed health
among Spanish older people living at home. J Epidemiol Community
Health. 1999; 53: 412-6.
12. World Health
Organization. Statistics Netherlands. Health interview surveys: towards
international harmonization of methods and instruments. Vol. 58.
Copenhagen: WHO Regional Office for Europe, WHO Regional Publications,
European; 1996.
13. Engel G. The need for a new medical model: a Challenge for biomedicine. Science. 1977; 196: 129-36.
14. Borrell-Carrio F, Suchman
AL, Epstein R. The bio-psychosocial model 25 years later: principles,
practice and scientific inquiry. Ann Fam Med. 2004; 2: 576-82.
15. Von Bertalanffy LV. Teoría general de los sistemas. México: Fondo de Cultura Económica; 1998.
16. Lee Y. The predictive
value of self assessed general, physical, and mental health on
functional decline and mortality in older adults. J Epidemiol Community
Health. 2000; 54: 123-9.
17. Ubel PA. What should I
do, doc?: Some psychological benefits of physician recommendations.
Arch Intern Med. 2002; 162: 977-80.
18. Blazer DG. How do you
feel about...? Health outcomes in late life and self-perceptions of
health and well-being. Gerontologist. 2008; 48: 415-22.
19. Wong R, Peláez M,
Palloni A. Autoinforme de health general en adultos mayores de
América Latina y el Caribe: su utilidad como indicador. Rev
Panam Health Publica. 2005: 17: 323-32.28.
20. Gómez JF, Curcio
CL, Matijasevic F. Autopercepción de health, presencia de
enfermedades y discapacidades en ancianos de Manizales. Rev Asoc Colomb
Gerontol Geriatr. 2004; 18: 706-15.
21. Parra DC, Gómez
LF, Sarmiento OL, Buchner D, Brownson R, Schimd T, et al., Perceived
and objective neighborhood environment attributes and health related
quality of life among the elderly in Bogotá, Colombia. Soc Sci
Med. 2010; 70: 1070-6.
22. Hambleton IR, Clarke K,
Broome HL, Fraser HS, Brathwaite F, Hennis AJ. Historical and current
predictors of self-reported health status among elderly persons in
Barbados. Rev Panam Health Publica. 2005; 17: 342-52.
23. Alves LC,
Rodrígues RN. Determinants of self-rated health among elderly
persons in São Paulo, Brazil. Rev Panam Health Pública.
2005; 17: 333-41.
24. Reyes-Ortiz CA,
Peláez M, Koenig HG, Mulligan T. Religiosity and self-rated
health among Latin American and Caribbean elders. Int J Psychiatry Med.
2007; 37: 425-43.
25. Department of Health.
2002. Guidance on the single assessment process for older people. HSC
2002/001; LAC (2002)1. London: Department of Health.
26. Bjorner JB, Tage SK,
Orth-Gomér K, Gösta T, Sullivan M, Westerholm P. Self-rated
health: a useful concept in research, prevention, and clinical
medicine. Stockholm: Ord & Form AB; 1996.33.
27.Ware JEJr, Sherbourne CD.
The MOS 36-item short-form health survey (SF-36) (I). Conceptual
framework and item selection. Med Care. 1992; 30: 473-83.
28. McHorney CA, Ware JEJr,
Raczek AE. The MOS 36-Item short-form health survey (SF-36): II.
Psychometric and clinical tests of validity in measuring physical
and mental health constructs. Med Care. 1993; 31: 247-63.
29. Lugo LH, García
HI, Gómez C. Confiabilidad del cuestionario de calidad de vida
en health SF-36 en Medellín, Colombia. Rev Fac Nac Health
Publica. 2006; 24: 37-50.
30. Eriksson I, Unden AL,
Elofsson S. Self-rated health. Comparisons between three different
measures. Results from a population study. Int J Epidemiol. 2001; 30:
326-33.
31. Jürges H, Avendano
M, Mackenbach JP. Are different measures of self-rated health
comparable? An assessment in five European countries. Eur J Epidemiol.
2008; 23: 773-81.
32. Seculi E, Fuste J,
Brugulat P, Junca S, Rue M, Guillen M. Percepción del state of
health en varones y mujeres en las últimas etapas de la vida.
Gac Sanit. 2001; 15: 217-23.
33. Hoeymans N, Feskens EJM,
Van den Bos GAM, Kromhout D. Measuring functional status: cross
sectional and longitudinal association between performance and
self-report (Zutphen Elderly Study 1990-1993). Clin Epidemiol. 1996;
49: 1103-10.
34. Liang J, Shaw BA, Krause
N, Bennett JM, Kobayashi E, Fukaya T, et al. How does self-assessed
health change with age? A study of older adults in Japan. J Gerontol B
Psychol Sci Soc Sci. 2005; 60: S224-32.
35. Idler EL. Age differences
in self-assessments of health: age changes, cohort differences, or
survivorship? J Gerontol Soc Sci. 1993; 548: S289-300.
36. Fries JF. Successful aging. An emerging paradigm of gerontology. Clin Geriatr Med. 2002; 18: 371-82.
37. Wong R. La
relación entre health y nivel sociodemográfico entre
adultos mayores: diferencias por género. En: Salgado de Snyder
V, Wong R, eds. Envejeciendo en la pobreza: género, health y
calidad de vida. México, DF: Instituto Nacional de Health
Pública; 2004. p. 97-122.
38. Palloni A, Pinto-Aguirre
G, Peláez M. Demographic and health conditions of ageing in
Latin America and the Caribbean. Int J Epidemiol. 2002; 31: 762-71.
39. Albala C, Lebrão
ML, León Díaz EM, Ham-Chande R, Hennis AJ, Palloni A, et
al. Encuesta Health, Bienestar y Envejecimiento (SABE):
metodología de la encuesta y perfil de la población
estudiada. Rev Panam Health Pública. 2005; 17: 307-22.
40. Wallace R, Herzog AR. Overview of the health measures in the Health and Retirement Study. J Hum Resour. 1995; 30: S84-107.
41. Baker M, Stabile M, Deri C. What do self-reported, objective, measures of health measure? J Hum Resour. 2004; 39: 1067-93.
42. Menéndez J,
Guevara A, Arcia N, León-Díaz EM, Marín C, Alfonso
JC. Enfermedades crónicas y limitación funcional en
adultos mayores: estudio comparativo en siete ciudades de
América Latina y el Caribe. Rev Panam Health Pública.
2005; 17: 353-61.
43. Leventhal H, Diefenbach
M, Leventhal EA. Illness cognition: using common sense to understand
treatment adherence and affect cognition interactions. Cogn Ther Res.
1992; 16: 143-63.
44. Ocampo JM, Romero N, Saa
HA, Herrera JA, Reyes-Ortiz CA. Prevalencia de las prácticas
religiosas, disfunción familiar, soporte social y
síntomas depresivos en adultos mayores. Cali, Colombia 2001.
Colomb Med. 2006; 37 (Supl 1): 26-30.66.
45. Blazer DG. Depression in late life: review and commentary. J Gerontol A Biol Sci Med Sci. 2003; 58: 249-65.
46. Lavretsky H, Kumar A.
Clinically significant non-major depression: old concepts, new
insights. Am J Geriatr Psychiatry 2002; 10(3):239 –55.
47. Anstey KJ, Luszcz MA,
Giles LC, Andrews GR. Demographic, health, cognitive, and sensory
variables as predictors of mortality in very old adults. Psychol Aging.
2001; 16: 3-11.
48. Hickey EM, Bourgeois MS.
Health-Related Quality of Life (HRQOL) in nursing home residents with
dementia: Stability and relationship among measures. Aphasiology. 2000;
14: 669-79.
49. Walker JD, Maxwell CJ,
Hogan DB, Ebly EM. Does self-rated health predict survival in older
persons with cognitive impairment? J Am Geriatr Soc. 2004; 52: 1895-900.
50. Lammi UK, Kivela SL,
Nissinen A. Predictors of disability in elderly Finish men. A
longitudinal study. J Clin Epidemiol. 1989; 42: 1215-25.
51. Idler EL, Kasl SV.
Self-ratings of health: do they also predict change in functional
ability? J Gerontol Soc Sci. 1995; 50B: S344-53.
52. Badley EM, Yoshida K,
Webster G. Disablement and chronic health problems in Ontario. Ontario
Health Survey 1990. Working Paper N° 5. Toronto: Ministry of
Health; 1993.
53. Lima-Costa MF, Firmo JO,
Uchoa E. The structure of self-rated health among older adults: the
Bambui health and ageing study (BHAS). Rev Saude Publica. 2004; 38:
827-34.
54. Heistaro S, Jousilahti P,
Lahelma E, Vartiainen E, Puska P. Self rated health and mortality: a
long term prospective study in eastern Finland. J Epidemiol Community
Health. 2001; 55: 227-32.
55. Murata C, Kondo T,
Tamakoshi K, Yatsuya H, Toyoshima H. Determinants of self-rated health:
Could health status explain the association between self-rated health
and mortality? Arch Gerontol Geriatr. 2006; 43: 369-80.
56. Benyamini Y, Levanthal
EA, Levanthal H. Self-assessments of health: What do people know that
predicts their mortality? Res Aging. 1999; 21: 477-500.
57. Idler EL, Russell LB,
Davis D. Survival, functional limitations, and self-rated health in the
NHANES I epidemiologic follow-up study, 1992. Am J Epidemiol. 2000;
152: 874-83.
58. Leinonen R, Heikkinen E,
Jylhä M. Predictors of decline in self-assessments of health among
older people: a 5-year longitudinal study. Soc Sci Med. 2001; 52:
1329-41.
59. Heistaro S, Laatikainen
T, Vartiainen E, Puska P, Uutela A, Pokusajeva S, et al., Self-reported
health in the Republic of North Karelia, Russia and in North Karelia,
Finland in 1992. Eur J Public Health. 2001; 11: 74-80.
60. Kaplan GA, Goldberg DE,
Everson SA, Cohen RD, Salonen R, Tuomilehto J, et al. Perceived health
status and morbidity and mortality: evidence from the Kuopio ischaemic
heart disease risk factor study. Int J Epidemiol. 1996; 25: 259-65.
61. Leinonen R, Heikkinen E,
Jylha M. Changes in health, functional performance and activity predict
changes in self-rated health: a 10-year follow-up study in older
people. Arch Gerontol Geriatr. 2002; 35: 79-92.
|