Factors associated with mortality through sepsis syndrome in children 31 days to 14 years of age. Hospital Universitario del Valle, Cali
Dolly Villegas, Enf, MSc1, Carlos Armando Echandía, MD, MSc2
1. Chief Epimemiology Hospital, Hospital Universitario del Valle, Cali. e-mail: dvillegas@huv.gov.co
2. Assistant Professor, Department of Pediatrics, School of Medicine, Faculty of Health, Universidad del Valle, Cali, Colombia. e-mail: cechandia@hotmail.com
Received for publication October 7, 2009 Accepted for publication August 31, 2010
SUMMARY
Objective: To determine factors associated with mortality by sepsis syndrome in children.
Methods: We performed an analytical study of cases and controls, which included patients between 31 days and 14 years of age, treated at Hospital Universitario del Valle in Cali, Colombia, with sepsis syndrome between 1999 and 2003. Information was gathered from medical records and books. The outcome variable was the status on discharge from hospital (alive or dead). All the dead children were verified in the hospital records and all the living children were confirmed alive four weeks after discharge. The exposure control variables were age, gender, origin, socioeconomic status, educational level of mothers, family order of the child, classification and origin of sepsis, nutritional status, underlying disease, presence and type of immunosuppression, invasive procedures, duration of surgery, broad-spectrum antibiotics, as well as preoperative, hospital and intensive care stay.
Results: We evaluated 110 cases and 110 controls, 79 with diagnosis of sepsis and 31 with septic shock. The cases had more days of evolution of the disease, higher proportion of family order of the child between third and fifth offspring, malnutrition, acquired immunosuppression, respiratory origin of sepsis, and shorter hospital stay and in intensive care. The logistic regression model showed that more days of disease progression (OR 1.05 CI 95% 1.01-1.10), and family order of the child (1.39 CI 95% 1.11-1.74), meant greater risk of dying from sepsis syndrome.
Conclusions: It must be insisted to the community of the importance of consultation and early diagnosis of any infectious process for rapid identification of the bacteria, allowing the introduction of specific treatment and referral according to severity level.
Keywords: Sepsis; Infant mortality; Protein malnutrition.
Factores asociados con mortalidad por síndrome de sepsis en niños entre 31 días y 14 años de edad. Hospital Universitario del Valle, Cali
RESUMEN
Objetivo: Determinar los factores asociados con mortalidad por síndrome de sepsis en niños.
Métodos: Se diseñó un estudio analítico de casos y controles, que incluyó pacientes de 31 días a 14 años de edad, atendidos entre 1999 y 2003 en el Hospital Universitario del Valle, Cali, con síndrome de sepsis. Se obtuvo información de las historias clínicas, de los libros de egreso y del anfiteatro. La variable desenlace fue el estado al egreso del hospital (vivo o muerto). Todos los niños muertos fueron verificados en los libros de defunciones del hospital y todos los vivos fueron confirmados cuatro semanas posteriores al egreso. Las variables de exposición de control fueron edad, género, procedencia, estrato socioeconómico, nivel educativo de las madres, orden familiar del menor, clasificación y origen de la sepsis, estado nutricional, enfermedad de base, presencia y tipo de inmunosupresión, procedimientos invasivos, duración de la cirugía, antibióticos de amplio espectro, estancia prequirúrgica hospitalaria y en cuidados intensivos.
Resultados: Se evaluaron 110 casos y 110 controles, 79 con diagnóstico de sepsis y 31 con choque séptico. Los casos tuvieron más días de evolución de la enfermedad, mayor proporción de orden familiar del menor entre tercero y quinto, de desnutrición, inmunosupresión adquirida, origen respiratorio de la sepsis y menor estancia hospitalaria y en cuidados intensivos. El modelo de regresión logística mostró que a más días de evolución de la enfermedad (OR 1,05 IC 95% 1,01-1,10) y orden familiar del menor (1,39 IC 95% 1,11-1,74), era mayor el riesgo de morir por el síndrome de sepsis.
Conclusiones: Insistir a la comunidad acerca de la importancia de la consulta y diagnóstico temprano de todo proceso infeccioso para la rápida identificación del germen, que permita la instauración del tratamiento específico y según severidad remisión a un nivel superior.
Palabras clave: Sepsis; Mortalidad infantil; Desnutrición.
One of the most complex infectious problems threatening the lives of pediatric and adult populations is sepsis syndrome: «the systemic inflammatory response to severe infection in an individual». Its diagnosis has increased within the last 25 years because of novel therapeutic advancements of chronic, debilitating, and malignant disease, as well as increasingly advanced surgical techniques, the development of cardiovascular surgery, and intensive care services that save thousands of lives and prolong the lives of high-risk and/or immunosuppressed patients, increasing susceptibility to infectious disease1-3.
In developing nations like Colombia, contribution to the disease is also made by medical services deficient in quality and quantity, tardy consultation or remission to a tertiary healthcare center, inadequate use of antibiotics, and high frequency of infectious gastrointestinal and respiratory diseases in the pediatric population1,4.
In spite of the great advancement in the knowledge of physiopathogenic mechanisms of sepsis, with respect to inflammatory response, standardization of the terminology when establishing diagnostic clinical criteria, attempts to modulate this exaggerated response, the availability of broad-spectrum antibiotics, and sophisticated support and critical care techniques, the rate of mortality has not changed1,3,5,6.
In a revision of 12,000 discharges per year, in children 31 days to 14 years of age, in Hospital Universitario del Valle (HUV) in the city of Cali, Colombia, we found a prevalence of sepsis at 4% and septic shock at 0.5%, with mortality of 42% and 80%, respectively. Through the present study, we sought to identify factors associated to mortality due to sepsis syndrome in children.
METHODS
An analytical observational study was designed of cases and controls, one case per control, in children 31 days to 14 years of age, cared for between 1999 and 2003 in HUV, reference center in the Colombian southwest for level III healthcare attention to patients from low socioeconomic levels. The following were inclusion criteria:
Sepsis: evidence of infection and the presence of two or more of the following: hyperthermia or hypothermia, tachycardia, tachypnea, leukocyte abnorma-lities, leukocytosis or leukopenia, neutrophilia, deviation to the left.
Severe sepsis: sepsis with the presence of one or more of the following: evidence of hypotension or hypoperfusion (capillary refill above 3 seconds), which responds quickly to administering of liquids, mental alterations, hypoxemia, oliguria (<0.5 ml/kg/h), metabolic acidosis.
Septic shock: severe sepsis with evidence of hypotension or hypoperfusion, which does not respond quickly to liquids administered and requires administration of inotropic medications. Exclusion criteria: children with multiple malformations or having incomplete information required for the study format.
Definition of the cases: patients 31 days to 14 years of age who died of sepsis syndrome, during a 5-year period 1999-2003 in HUV in Cali.
Definition of controls: patients 31 days to 14 years of age who survived (alive up to 4 weeks after discharge) sepsis syndrome during a 5-year period 1999-2003 in HUV.
Sample size: we used the Epi-Info 6.04 statistical package, with a 10% probability (P1) of exposure expected in the live discharges, P2 of 15% exposure in the dead subjects, permitted type I and type II errors of 5% and 10%, respectively, a power of 90%, a minimum OR of 1.5, one case per control, we calculated a sample size of 110 cases and 110 controls.
Bearing in mind that during the period from 1995 to 2003 there were 1176 patients with sepsis syndrome in HUV, of which 72% were sepsis and 28% septic shock, of the total of 220 patients needed for the study 79 cases and 79 controls were taken with sepsis and 31 cases and 31 controls with septic shock.
Measurements: the outcome variable was the status of discharge from the hospital (alive or dead). All the dead children were verified in deaths registration books in HUV and all the live cases were confirmed via home visits (10%), telephone calls (34%), and controls after discharge in outpatient pediatric consultation (56%).
The control exposure variables were: age, gender, ethnicity, socioeconomic level, origin, motherís educational level, and childís family order. Additionally, there was classification and origin of the sepsis syndrome, immunization and nutritional status, underlying disease, presence and type of immunosuppression, weight, temperature, cardiac and respiratory frequencies, blood pressure, diuresis, capillary refill, invasive procedures, surgery, duration of surgery, along with pre-surgical, hospital, and ICU stay, and broad-spectrum antibiotics.
Description and management of information: one of the authors (DVA) reviewed admittance records of all the pediatric services at HUV from 1999 to 2003, looking for children with sepsis syndrome; then requested 720 clinical charts from the department of statistics, of which 47 were discarded (25 did not correspond to the age and 22 to the diagnosis); of the 671 remaining we obtained the list to randomly make the sample.
The format designed to gather the information was subjected to a validation test to observe its consistency. Two pediatricians applied the test in alternate manner in two clinical histories with diagnosis of sepsis syndrome. This validation found disagreement in sepsis syndrome diagnosis upon admittance, socioeconomic level and family order, which permitted improving the instrument. Thereafter, a pilot test was conducted with a sample of 10 clinical histories to verify the quality of the information obtained. Through this test, we decided not to include size or state of consciousness, given that they were not referred to in 8 of the clinical histories.
All the information gathered from the histories, by a previously trained pollster who was unaware of the study objectives, was digitized on to data base created in the Epi-Info 6.04 statistical package and then edited to find the missing data and kept within the logical range.
Analysis plan: a description of the study population was conducted. To describe the continuous variables, we used averages, means, ranges, and standard deviation. The discrete variables were obtained via absolute and relative frequencies. Baseline characteristics were compared between patients from Cali and outside of Cali and between cases and controls, using Fischerís exact test or the X2 test for categorical variables, and U Mann Whitney test for continuous variables.
A bivariate analysis was carried out, examining the relationship of each of the control exposure variables with the status upon discharge from the hospital (alive or dead) to determine which were associated and the apparent magnitude of their association.
Linearity among each of the independent continuous and outcome variables was evaluated, due to a logistic transformation and to a graphic of point dispersion. If they did not show linearity, they were dichotomized in their mean and entered the model as indicator variables. The categorical independent variables associated with the outcome entered the model as indicator variables. The presence of co-linearity between the independent variables was explored via the correlation matrix, according to Spearmanís test.
Finally, a multivariate analysis was performed using an association logistic regression model, starting with a model including all the independent variables associated to the outcome and, through the Wald statistical test, it was decided whether to include or eliminate each of the variables.
Ethical aspects. According to Scientific, Technical, and Administrative Norms for Research on Humans, Resolution N° 8430 of 1993 from the Colombian Ministry of Health, this study was classified without risk and was evaluated and approved by the Ethics Committee at HUV.
RESULTS
We evaluated 110 cases and 110 controls, 79 with sepsis diagnosis and 31 with septic shock, seen at HUV between January 1999 and June 2003. Fourteen patients were replaced, 6 cases and 8 controls, because of incomplete information.
A total of 58% of the population were male, 45% with incomplete immunizations, 42% with malnutrition (51% classified grade I), and 23% with immunosuppression (78% acquired). Regarding the mothers, 46% had secondary education; 97% of the patients were from low socioeconomic level and 59% were from outside of Cali.
Diagnosis of the sepsis syndrome was done upon admittance in 179 (81.4%) children and the rest during hospitalization. The origin of the sepsis syndrome upon admittance was mainly respiratory (43.6%) and gastrointestinal (40%), followed by staphycoccemia (10.6%).
In patients with diagnosis for sepsis syndrome during hospitalization (41), nosocomial respiratory entities (50%) predominated as its origin, followed by gastrointestinal causes (27%), staphycoccemia (12%), urinary infection associated to catheterization (7%), and sepsis associated to central catheter (5%).
Septic shock evolved in 6% of the children with sepsis. The evolution of the disease was on the average of days (1-99) and the hospital stay was of 17 days (1-197).
Only 59 blood cultures (26%) blood cultures were taken, of which 73% were positive, with staphylococcus as the most frequent germ, followed by Klebsiella and meningococcus. Eight (18.6%) of the positive blood cultures were reported as resistant in the antibiogram. There were 21 urine cultures taken (9.5%), of which 28.6% were positive, with meningococcus as the most frequent germ, followed by Candida. One of the urine cultures was reported resistant.
When comparing baseline characteristics between those from Cali (41%) and those from outside (59%), we found in the latter a greater mean age (39.5 months versus 25 months, p=0.05), greater percentage of girls (60% against 45%, p=0.04), and longer hospital stay (average 19 days against 13 days, p=0.02) than those from Cali. Their mothers had lower educational levels (secondary education 34% vs. 62%, p=0.00). No differences were found regarding days of evolution of the disease.
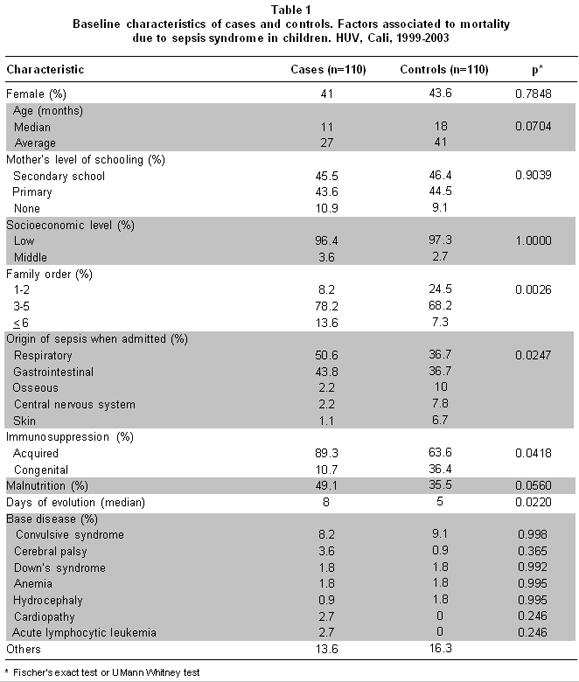
When comparing the baseline characteristics between cases and controls, no differences were found regarding gender, age, ethnicity, origin, socioeconomic level, and motherís education, along with vaccination status, immunosuppression, and underlying disease (Table 1).
In the 41 children with diagnosis during their hospitalization, there also were no differences in cases and controls regarding central catheter (47% vs. 30%, p=0.403), catheterization (24% vs. 10%, p=0.409), orotracheal tube (43% vs. 60%, p=0.432), prior surgery (38% vs. 35%, p=0.484) and broad-spectrum antibiotics (34% vs. 65%, p=0.086).
Differences were found related to cases having more days of evolution of the disease, higher family order of the child, greater proportion of the origin of the sepsis in the respiratory system, acquired immunosuppression and malnutrition, as well as lower hospital stay in critical care and pre-surgery, than the controls (Table 1).
Linearity was found with the outcome variable, during hospital stay, days of evolution of the disease, and the childís family order. Greater family order and more days of evolution of the disease indicated greater mortality (Graphics 1 and 2).
The variables of age, pre-surgical time, surgical time, and stay in ICU, which did not show linearity, were dichotomized in their mean and along with type of immunosuppression and malnutrition were converted into indicator variables.
Co-linearity was found in the correlation matrix between malnutrition and immunosuppression and between hospital stay and surgical time, prompting us to include malnutrition and hospital stay in the model.
A regression logistic model was created with the variables of days of evolution of the disease, childís family order, hospital stay, pre-surgical time; and age, malnutrition, stay in ICU were included because they were considered important control risk factors. By following the step-by-step technique, we obtained the model that best explained the risk of dying due to sepsis syndrome: greater number of days of evolution of the disease (OR 1.05 CI 95% 1.01-1.10) and childís family order (1.39 CI 95% 1.11-1.74), led to greater risk of dying due to sepsis syndrome (Table 2).
DISCUSSION
The factors associated with death due to sepsis syndrome, identified in this retrospective study, were the days of evolution of the disease and the childís family order.
As in most medical situations, it must be stressed upon the community and upon healthcare personnel about the measures to prevent the development of sepsis: the importance of early consultation and diagnosis of every infectious process for the rapid identification of the bacteria, virus, or fungus, which permits the opportune instauration of specific treatment and, according to the severity, remission to a higher healthcare level, controlling the whole chain of inflammatory response, which if not interrupted, may lead children to a state of greater risk upon their lives7,8. Frequently, this opportunity is affected by difficulties in being seen at in healthcare centers and/or delays in consulting from the parents or legal guardians, which leads to many hours or days transpiring since the start of the process, overshadowing the prognosis9. Carrillo et al.1, reported that chronic malnutrition, deficient medical services, inadequate use of antimicrobial medications and late remission to level three attention, contribute to the development of sepsis and septic shock. In this study, we found that greater number of days of evolution of the disease increases the risk of dying due to sepsis (OR 1.05 CI 95% 1.01-1.10), with a small but significant effect (Graphic 1).
Although we did not find this type of data in the literature reviewed, we sought to know the influence of the childís family order and the outcome of sepsis syndrome. This study found that greater family order of the child indicated greater risk of dying due to sepsis syndrome (1.39 CI 95% 1.11-1.74) (Graphic 2), possibly because greater care and attention the mother devotes to the newborn or the to the youngest lactating children in the home means paying less attention to the older children.
It is possible that prolonged hospitalizations are due to more serious medical conditions, making patients more labile to the infection. Brun et al., reported that with one day of hospitalization the percentage of infection is 1.1%, with one week it is 2%, and if the patient remains hospitalized for more than two weeks it is 4.3%4. In this study, a selection bias was found, given that the group of dead children had fewer days of hospital stay and in ICU, a result influenced by the severity of the sepsis: these children were admitted in very serious condition, requiring care in ICU, but died quite quickly; 65% of the deaths occurred between the first and fourth day of admission to the hospital.
In spite of the low use of cultures in this group of children, only 26% blood cultures and 9.5% urine cultures, we obtained another finding agreeing with the literature, testing positive (73%) in blood cultures, which was above the 60% reported by Butt8 in children with sepsis and predominance of the staphylococcus aureus, as the most frequently associated germ, reported by the study on «the epidemiology of the sepsis» conducted in the United States from 1979 to 200010 and by Han et al.2
In the current study we found no association with variables recognized in world literature, with the risk of dying of sepsis condition, like the age of the child, malnutrition, the motherís level of schooling, and the pre-surgical stay.
Several authors have considered extreme ages as risk factors for falling ill and dying. The study «Sepsis in the lactating infant» by Hernández et al.11, manifested that most affected were children younger than two years of age, because they cannot produce killer cells, becoming more susceptible to severe infections7,12,13. In the current study, the ages of cases were lower than those of the controls (11 months versus 18.5 months, p=0.07), but in the regression model age was not found related to the risk of dying due to sepsis. One possible explanation may be that we took a rather broad age range (from 31 days to 13 years of age).
The findings in our study were also not consistent with the world nutritional literature14,15, which places malnutrition as a strong risk factor for mortality due to sepsis. A study analyzing clinical, epidemiological, and microbiological data in systemic infections in children hospitalized in Malawian, Africa, to determine some clinical indication that may identify those in high risk of dying, found six times greater risk of dying among malnourished children with adequate weight5, recommending facilities for admission of these children to ICU for their proper management.
In the current study, we found a greater percentage of malnourished children in the cases than in the controls (49% vs. 35.5%, p=0.05), but in the regression model this was not found associated to the risk of dying due to sepsis.
Numerous authors have shown association between low schooling levels of the mothers and high rates of mortality of their children. An epidemiological surveillance study of infant mortality due to diarrheal disease in Cali16 found that of 100 children who had died due to diarrhea, that 82.5% of their mothers had not completed primary school or had only finished primary school. In our study, the proportion of schooling in the mothers was similar, 46% of the mothers of the cases and the controls had secondary education.
The pre-surgical stay and surgical time were considered variables of importance according to Cruse and Ford, who reported the relationship between pre-surgical stay and the risk of infection, explained by the increased bacterial colonization and resistance during the hospitalization and by the severity of the associated disease17. Also, the duration of the surgery is related to contamination, greater tissue damage, diminished local resistance, and effect of the prophylactic antibiotic, duplicating the risk of infection with each hour of surgery. In this study, pre-surgical stay and time of surgery revealed statistical association with mortality, but when considering the pre-surgical stay with other variables in the logistic regression model, it did not explain the probability of dying due to sepsis syndrome.
In the 41 (19%) patients who acquired the sepsis syndrome during hospitalization, we analyzed factors like venous approach, mechanical ventilation, surgical intervention, stay in ICU, and other invasive procedures like central catheter and catheterization, without finding association with risk of dying due to sepsis. Some 88% of these patients were in ICU prior to sepsis diagnosis. Data derived from different third-level healthcare centers suggest that there are 3 to 6 deaths in every 10 patients suffering septic shock while in ICU18. In our current study, the group of dead patients had lower hospital and ICU stays because of the greater compromise and severity of the disease upon admission.
The strengths of this study were the validation of the questionnaire applied, first by two pediatricians in emergency service and then in a pilot study with 10 clinical histories and that all the living children were confirmed alive four weeks after discharge. Weaknesses of the study lie in that most of the information was taken from clinical histories in the Institution, constructed upon attendance with information deficit and no evaluation of confusion variables.
CONCLUSIONS
Conflict of interest. None of the authors has conflicts of interest related to this study.
ACKNOWLEDGEMENTS
We thank doctor Guillermo Llanos (RIP) for his outstanding collaboration, support, and accompaniment as director of this thesis.
REFERENCES
1. Carrillo HA, Santos JI. Sepsis y choque séptico. En: Rodríguez R, Velásquez L, Valencia P, Nieto J, Serrano A (eds.) Urgencias en pediatría. 4a ed. México, DF: Interamericana, McGraw Hill; 1996. p. 183-209.
2. Han YY, Carcillo J, Dragotta M. Early reversal of pediatric- neonatal septic shock by community physicians is associated with improved outcome. Pediatrics. 2003; 112: 793-99.
3. Bennet NR. Actualización sobre cuidados intensivos pediátricos. Pediatría y atención crítica. El Hospital. 2000; 56: 12-33.
4. Brun-Buisson C, Doyon F, Carlet J, Dellamonica P, Gouin F, Lepoutre A et al. Incidence, risk factor and outcome of severe sepsis and shock septic in adults. A multicenter prospective study in intensive care units. JAMA. 1995; 274: 968-74.
5. Norton EB, Archibald LK, Nwanyanww OC, Kazembe PN, Dobbie H, Reller LB et al. Clinical predictors of bloodstream infections and mortality in hospitalized Malawian children. Ped Infect Dis J. 2004; 23: 145-51.
6. Torres M. Enfoque del niño con sepsis. En: Roa J, Echandía CA (eds.) Emergencias y urgencias en pediatría. 2a ed. Cali: Aspromédicas; 2001. p. 193-209.
7. Rodríguez MA, López C, Arredondo JL, Gutiérrez P, Sánchez F. Morbilidad y mortalidad por sepsis neonatal en un hospital de tercer nivel. Salud Publica Mex. 2003; 45: 15-21.
8. Butt W. Septic shock. Pediatr Clin North Am. 2001; 48: 601-24.
9. Cifuentes Y. Síndrome de sepsis. En: Rojas E, Sarmiento F (ed.) Pediatría. diagnóstico y tratamiento. 2a ed. Bogotá, DC: Celsus; 2003. p. 237-42.
10. Martin GS, Mannino DM, Eaton S, Moss M. The epidemiology of sepsis in the United States from 1979 through 2000. N Engl J Med. 2003; 348: 1546-54.
11. Hernández I, Causa N, Vásquez J, Díaz B. Sepsis del lactante. Características clínicas y epidemiológicas en Cuba. Monografias.com. (monografía en línea) La Habana, 2000 [fecha de acceso septiembre de 2009]. URL disponible en: www.monografias.com/trabajos14/sepsis-lactante/sepsis-lactante.html
12. Gómez DA. Factores de riesgo asociados a infecciones. En: Navarrete NS, Muñoz HO, Santos PJI (eds.). Infecciones intrahospitalarias en pediatría. México, DF: McGraw Hill Interamericana; 1998. p. 46-53.
13. The WHO Young Infants Study Group. Clinical prediction of serious bacterial infections in young infants in developing countries. Pediatr Infect Dis J. 1999; 18: S23-S31.
14. Rice AL, Sacco L, Hyder A, Black RE. Malnutrition as an underlying cause of childhood deaths associated with infectious diseases in developing countries. Bull WHO. 2000; 78: 1207-21.
15. Schofield C, Ashworth A. Why have mortality rates for severe malnutrition remained so high? Bull WHO. 1996; 74: 223-9.
16. Concha A, Melo LM, Korgi MD, Franky M, Delgado F, Holguín JA. Vigilancia epidemiológica de la mortalidad por enfermedad diarreica en menores de 5 años en Cali. 1990 -1995. Colomb Med. 1995; 26: 125-31.
17. Cruse PJ, Ford R. The Epidemiology of wound infection. A ten year prospective study of 62 939 wounds. Surg Clin North Am. 1980; 60: 27-40.
18. Santillán MA, Muñoz J. Bacteremia en terapia intensiva. Rev Med IMSS. 1994; 32: 351-4.