Clinical and epidemiological characteristics of pediatric patients with positive serology for Mycoplasma pneumoniae, treated in the third level hospital from 2006 to 2008
Margarita María Suárez, MD1, Mussatyé Elorza, MD2, Jorge Hernando Donado, MD3, Luis Alfredo Londoño, MD4, David Andrés Espinal, MD5
1. Pediatric Resident Physician, Universidad Pontificia Bolivariana, Medellín, Colombia. e-mail: margaralema@hotmail.com
2. Pediatric Physician, Pablo Tobón Uribe Hospital, Resident Pediatric Intensive Care, CES, Medellín, Colombia. e-mail: mussatye@hotmail.com
3. Clinical Epidemiology Physician, Pablo Tobón Uribe Hospital. Full Professor, Universidad Pontificia Bolivariana, Medellín,
Colombia. e-mail: jdonado@hptu.org.co
4. Physician, Universidad Libre Seccional, Cali, Colombia. e-mail: lulondono@hotmail.com
5. Pediatric Physician, Chief Department of Pediatrics, Pablo Tobón Uribe Hospital, Medellín, Colombia. e-mail: despinal@hptu.org.co
Received for publication February 16, 2010 Accepted for publication September 20, 2010
SUMMARY
Introduction: Infection by Mycoplasma pneumoniae is becoming more frequent at younger ages. It appears as a generally benign and unspecific clinical condition of respiratory symptoms and sometimes responsible for a broad spectrum of extrapulmonary manifestations.
Objective: To describe demographic, clinical, laboratory, and treatment characteristics of pediatric-age patients with positive serology for M. pneumoniae diagnosed at the Pablo Tobón Uribe Hospital (HPTU) during the 2006-2008 period.
Materials and methods: Observational, retrospective study, which describes the demographic, clinical, laboratory, and treatment characteristics of patients from 1 month to 14 years of age with positive IgM for M. pneumoniae seen at HPTU during September 2006 and November 2008.
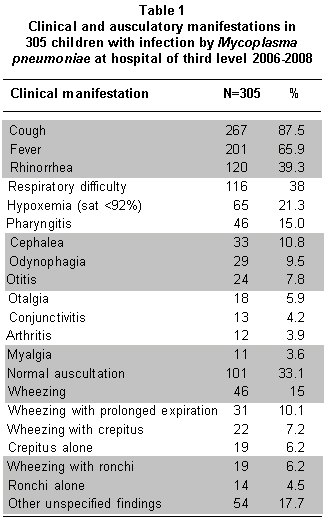
Results: We reviewed 305 clinical charts of patients with positive IgM for M. pneumoniae. The average age was 5.15 years ± 3.62 SD. Cough (87.5%), fever (65.9%), rhinorrea (39.3%), and respiratory difficulty (38%) were the most frequent clinical findings. Extrapulmonary compromise was mainly manifested in the skin (12.8%), the central nervous system (CNS) (3.6%), and osteomuscular system (3.9%). Auscultation and thoracic X-ray were normal in 33.1% and 30.8% of the patients, respectively. Episodes of asthma exacerbation were related to infection by Mycoplasma in 35% of the cases. A total of 51% of the patients required hospitalization with an average stay of seven days. All the patients received antibiotic treatment; clarithromycin (75.8%) was the antibiotic of choice.
Conclusion: Infection by M. pneumoniae has a broad range of clinical manifestations, requiring a high index of clinical suspicion and an active search for extrapulmonary compromise given that in our realm there is no specific diagnostic method for the acute infection.
Keywords: Mycoplasma pneumonia; Pneumonia; Extrapulmonary manifestations; Children.
Colomb Med. 2011; 42: 138-43
Características clínicas y epidemiológicas de pacientes pediátricos con serología positiva para Mycoplasma pneumoniae, atendidos en un hospital de tercer nivel durante el período 2006-2008
RESUMEN
Introducción: La infección por Mycoplasma pneumoniae es cada vez más frecuente a edades tempranas. Se presenta como un cuadro clínico de síntomas respiratorios generalmente benigno e inespecífico y en ocasiones es reponsable de un amplio espectro de manifestaciones extrapulmonares.
Objetivo: Describir las características demográficas, clínicas, de laboratorio y el tratamiento de pacientes en edad pediátrica con serología positiva para M. pneumoniae diagnosticados en el Hospital Pablo Tobón Uribe (HPTU) durante el período 2006-2008.
Materiales y métodos: Estudio observacional, retrospectivo, que describe las características demográficas, clínicas, de laboratorio y tratamiento de pacientes de 1 mes a 14 años de edad con IgM positiva para M. pneumonie atendidos en el HPTU entre septiembre de 2006 y noviembre de 2008.
Resultados: Se revisaron 305 historias clínicas de pacientes con IgM positiva para M. pneumoniae. La edad promedio fue 5.15 años ± 3.62 DE. La tos (87.5%), fiebre (65.9%), rinorrea (39.3%) y dificultad respiratoria (38%) fueron los hallazgos clínicos más frecuentes. El compromiso extrapulmonar se manifestó sobre todo en piel (12.8%), sistema nervioso (3.6%) y sistema osteomuscular (3.9%). La auscultación y la radiografía de tórax fueron normales en 33.1% y 30.8% respectivamente. Los episodios de exacerbación del asma se relacionaron con infección por Mycoplasma en 35% de los casos. Del total de niños, 51% necesitó hospitalización con un promedio de estancia de 7 días. Todos los pacientes recibieron tratamiento antibiótico, siendo el de elección claritromicina (75.8%).
Conclusión: La infección por M. pneumoniae posee una amplia gama de manifestaciones clínicas que requiere un alto índice de sospecha clínica y una búsqueda activa de compromiso extrapulmonar porque en Colombia no se cuenta con un método diagnóstico específico para la infección aguda.
Palabras clave: Mycoplasma pneumoniae; Neumonía; Manifestaciones extrapulmonares; Niños.
Colomb Med. 2011; 42: 138-43
In recent decades, respiratory infections have surpassed diarrhea as the main cause of morbidity in developing nations. Particularly, Mycoplasma pneumoniae has been shown to be a frequent cause of pneumonia in children and young adults; although diagnosis at younger ages has recently increased1-4.
Mycoplasma pneumoniae was first described in humans in 1942 by Eaton et al.1 It is an extracellular bacterium from the Mycoplasmataceae family, which is exclusively human and has universal distribution2. It is characterized for lacking a cell wall3 and not responding to the Gram staining.
The presentation of the infection is noted in epidemiological cycles every 3-5 years, with a frequency of 2 cases/1000 individuals/year5-8. In our realm, the frequency of infection by this microorganism is not well established. In the United States and Europe, it is responsible for up to 40% of community-acquired pneumonias (CAP) and 18% of pneumonias requiring hospitalization2,9-12. In Asia and Africa, it has been reported that 44% and 34% of the CAP in children are caused by M. pneumoniae. Latin American studies reported a prevalence of CAP due to Mycoplasma pneumoniae of 15% and 7% in Argentina and Panamá, respectively9.
Infection due to M. pneumoniae is considered benign and self-limited; it may be asymptomatic in 20% of the cases3,11 or run its course with extrapulmonary manifestations (meningoencephalitis, polyneuropathy, myelitis, arthritis, vasculitis, hemolytic anemia) in 15 to 25% of the cases1.
The immune response is manifested by the rapid production of antibodies responding to the organism's protein and glycolipid antigens, with a maximum concentration reached in 3 to 6 weeks and a decrease starting after 4 to 6 months11.
We described the epidemiological, clinical, laboratory, and treatment characteristics of patients with positive IgM for M. pneumoniae in the pediatric service at Pablo Tobón Uribe Hospital (HPTU) in the city of Medellín, Colombia during period between September 2006 and November 2008.
MATERIALS AND METHODS
This was an observational, retrospective study describing the epidemiological and clinical characteristics, along with laboratory results and treatment of pediatric-age patients (1 month to 14 years of age) with positive serology for M. pneumoniae in Pablo Tobón Uribe Hospital from September 2006 to November 2008.
During the study period, 457 positive IgM results for M. pneumoniae were included for patients between 1 month and 14 years of age. A total of 152 patients were excluded; 17 because their age was outside the range of the study, 90 had incomplete information, and 45 had no hospital records at the Institution. We reviewed 305 clinical charts and the information was recorded onto a previously designed format, which included demographic characteristics, clinical manifestations, imaging, laboratory results, and treatment.
The information gathered was tabulated onto a data base on Microsoft Excel® 2007, and exported to the SPSS version 15.0 statistical package (Chi IL) to present the results as mean and standard deviations.
The research was carried out according to Resolution N° 008430 of 1993 by the Ministerio de la Protección Social de Colombia, which establishes the scientific, technical, and administrative norms for health research. The Research and Ethics Committee at HPTU approved the research work, and steps were taken to protect the patients' identities and dignity and that of their families. The study is classified as research free of risk, given that no action is taken on the patients and only a documentary and retrospective revision is made.
RESULTS
Distribution by gender was 148 girls (48.5%) and 157 boys (51.5%); the age range was between 1 month and 14 years, with a mean of 5.15 ± 3.62 SD (4-year median). Some 95% of the patients were from the city of Medellín and its metropolitan area and 5% were from the rural area of the department of Antioquia.
A total of 63% of the patients attended school and only 35% had a history of asthma. Regarding the clinical condition at the time of consultation, we found a variable evolution, with a symptom onset median of 4 days (range from 1 to 150 days).
Cough was the most frequent symptom (87.5%), followed by fever (66%), rhinorrea (39.5%), and respiratory difficulty (38%) (Table 1). Other symptoms reported were pharyngitis (15%), cephalea (11%), odynophagia (9.5%), otitis (8%), otalgia (6%), conjunctivitis (4.3%), arthralgias (4%), and myalgia (3.6%) without significant difference in the frequency of presentation in the different age groups. Neurological symptoms were detected in 11 (3.6 %) patients, among which convulsions (27%), polyneuropathy (18%), and encephalopathy (9%) were the most frequent. Cutaneous manifestations were reported in 12.8% of the cases: exanthema (74.4%), wheal (5%), rash (2.6%), and vesicles (2.6%).
Pulmonary auscultation was normal in 33.1% of the patients. Among the abnormal findings there were only sibilance in 15% and a combination of pulmonary noise in 45% of the patients (Table 1).
Upon admission, hemoleukogram was requested from 241 patients (78.6%), where the leukocyte average was 11.488/mm3 and the differential was found normal in most patients. The C reactive protein (CRP) was carried out in 58% of the patients, with a median of 1.4 mg/dl (ranging from 0 to 39 mg/dl). Thoracic X-rays were ordered on 201 patients, 62 radiographs were reported normal (32%) and among the abnormal findings, the most frequent were interstitial infiltrates (28%) and air trapping (11%), (Table 2). Other diagnostic aids were requested from 58 patients; computerized axial tomography (CAT) of paranasal sinuses presented abnormal findings in 63% of the cases. Electromyography, skin biopsy, and cerebrospinal fluid (CSF) exam were requested from less than 1% of the patients.
A total of 51% of the patients were hospitalized, 10% in the special and intensive care unit. Supplementary oxygen was required for 33% of the patients and 1.3% needed mechanical ventilation. The average hospital stay was of 7 days with an interval between 1 and 137 days. Clinical records revealed droplet isolation in 134 (45.5%) of the cases. All the patients received antibiotic treatment; the antibiotic of choice was Clarithromycin (75.7%), followed by erythromycin (16.1%) and azithromycin (8.2%). Doctors ordered bronchodilators for 80% of the patients, steroids for 66% (systemic 36%, inhaled 36%, and both ways of administering 28%), analgesics and antipyretics for 47.3%, and antihistamines for 24.5% of the patients (Table 3).
RESULTS
Mycoplasma pneumoniae has always been considered one of the main causes of respiratory infection in school-age populations. However, during the last two decades it has been more frequently identified at earlier ages12,14,15. In the current study, 63% of the patients with positive serology were less than five years of age and coincidentally the same percentage was of school age.
In general, manifestations of infection by this microorganism are variable and unspecified and the clinical condition has a gradual onset during days or months11,16. Regarding the evolution of symptoms, the findings in this study do not differ with that reported in the literature and the frequency is similar to that found by Waites et al.13, with respect to fever, cough, compromise of the general status, cephalea, and odynophagia6,12,15.
Infection by M. pneumoniae has a known role as triggering of asthmatic exacerbations in children17-19, Biscardi et al.2, reported infection by this microorganism as the cause of 50% of acute crisis of patients with a history of asthma and as a risk factor for unfavorable evolution in 20% of these2. In this investigation, 35% of the patients had a history of asthma but the infection was not identified as triggering the crisis because such was not one of the objectives of the study.
Although respiratory manifestations predominate in acute infection by M. pneumoniae, extrapulmonary compromise is reported in up to 25% of the cases, occurring even after the respiratory disease or in the absence of such10,13,15,19,21. We noted the skin as the most frequently committed organ at extrapulmonary level, followed by the affectation of the CNS and the osteomuscular system.
Findings of physical exam are unspecific. In this work, we found normal auscultation in 33% of the patients and sibilance in 15%; however, Othman et al.11,20, describe that sibilance is found in over a third of the CAP caused by M. pneumoniae in hospitalized children11-21.
Isolating M. pneumoniae via oropharyngeal or nasopharyngeal aspirate culture is considered the method of choice for the diagnosis of acute infection. Its usefulness is limited in clinical practice because it requires from 10 to 14 days. Polymerase chain reaction (PCR) is one of the alternatives in confirming the diagnosis8,10,22, but it is not available in our realm.
The IgM for Mycoplasma may be used via the enzimoinmunoensayo22 technique, but this requires comparison of paired sera to confirm the diagnosis of acute infection. In the current investigation, the technique used in measuring IgM (immunocard R Mycoplasma) has a specificity of 90 ± 3% and a sensitivity of 88 ± 6%, but in positive values which do not distinguish between current or recent infection (<12 months of evolution). Souliu et al.11, suggest that for the diagnosis of M. pneumoniae as etiology of a respiratory condition, IgM through the ELISA method should be confirmed via PCR or culture; increased immunoglobulin M in paired samples or levels of IgG >400 U/ml21,23. Our study did not conduct diagnostic confirmation because of the retrospective character and because these techniques were not available in the clinical practice. Long-term persistence of seropositivity in spite of adequate antibiotic treatment of the infection4,10,11,24 hinders the interpretation of the results because of the high percentage of false positives.
We found no specific alterations in para-clinical exams, which permit distinguishing the infection by M. pneumoniae from that produced by other microorganisms. The leukocyte count was normal or slightly high9,16 with differential and PCR within the normal range12,16. The thoracic X-ray reveals a variety of patterns that hinder diagnostic orientation merely through images, finding it normal in 31% of the cases2,6,11,12,16,21.
In different observational studies, hospitalization in infection by M. pneumoniae is required in approximately 20% of the cases2,12,13. Perhaps in our realm, the report that over half of the patients require hospitalization may be due to the possibility of out-patient follow up and treatment cannot be assured.
Infection by M. pneumoniae is often self-limited; with improvement of symptoms within the first 10 days2,16. In spite of this, it was found that all the patients in this study received antibiotic treatment. Some literature reviewed justify antibiotic treatment, asseverating that it limits morbidity by pneumonia, shortens the duration of the symptoms, and decreases the frequency of recurrent sibilance episodes, although it does not reduce the risk of transmission9.
Although M. pneumoniae is susceptible to antibiotics like tetracycline and quinolones, it is treated as a first therapeutic option with macrolides10-12,15,16 because of its safety during pediatric age, clinical and radiological improvement, along with the microbiological erradication2,17,25. The symptomatic treatment (non-antibiotic) does not reveal sufficient evidence regarding improvement, duration of symptoms, and time of hospital stay of patients with non-complicated infections.
In conclusion, infection by M. pneumoniae has a broad variety of manifestations, which turn out to unspecific to reach a clinical diagnosis. A high index of suspicion is required to avoid mainly extrapulmonary complications, which are the most serious. Hence, to confirm the infection and optimize the treatment regarding the rational use of antibiotics, it is indispensable to have a method with a high level of sensitivity and specificity for which IgM, without comparing labels in paired sera, is not suitable. Based on this, we suggest the need to conduct a prospective study to compare the positive results of IgM for M. pneumoniae and PCR for the diagnosis of acute infection.
Conflict of interest. None of the authors has conflicts of interest related to this study.
REFERENCES
1. Sánchez-Vargas FM, Gómez-Duarte OG. Mycoplasma pneumoniae - an emerging extra-pulmonary pathogen. Clin Microbiol Infect. 2008; 14: 105-17.
2. Alves-Vervloet L, Christophe M, Moreira-Camargos PA. Infection by Mycoplasma pneumoniae and its importance as an etiological agent in childhood community-acquired pneumonias. Braz J Infect Dis. 2007; 11: 507-14.
3. Gendrel D, Biscardi S, Marc E, Moulin F, Iniguez JL, Raymond J. Mycoplasma pneumoniae, community-acquired pneumonia and asthma. Arch Pediatr. 2005; 12 (Suppl 1): S7-11.
4. Matas L, Molinos S, Fernández G, González V, Ausina N. Diagnóstico serológico de las infecciones por Mycoplasma pneumoniae. Enferm Infecc Microbiol Clin. 2006; 24: 19-23.
5. Espinosa-Gimeno A, Martínez-Alfaro E, Meseguer-Ruiz V, Solera-Santos J. Infección por Mycoplasma y Chlamydia. Medicine. 1998; 7: 3687-92.
6. American Academy of Pediatrics. Mycoplasma pneumoniae infections. In: Pickering LK (ed.) Red Book: Report of the Committee on Infectious Diseases. 27th ed. Elk Grove Village: American Academy of Pediatrics; 2006. p. 441-3.
7. Ferwerda A, Moll HA, de Groot R. Respiratory tract infections by Mycoplasma pneumoniae in children: a review of diagnostic and therapeutic measures. Eur J Pediatr. 2001; 160: 483-91.
8. Bébéar CM. Pathogenesis and laboratory diagnosis of Mycoplasma pneumoniae infections. Arch Pediatr. 2008; 15: 1253-6.
9. Paul MA, García C, Vega-Briceño L. Infección por Mycoplasma pneumoniae. Rev Neumol Pediatr (on line) 2007 (Access 19 June 2009); 2: 140-46. URL available in: http://www.neumologia-pediatrica.cl.
10. Bologna R. Mycoplasma pneumoniae: lo que nos queda por conocer. Arch Argent Pediatr. 2008; 106: 3-5.
11. Paul MA, Vega-Briceño L, Potin M, Ferrés M, Pulgar D, García C, et al. Características clínicas de la enfermedad respiratoria causada por Mycoplasma pneumoniae en niños hospitalizados. Rev Chilena Infectol. 2009; 26: 343-9.
12. Grunfeld de Viú J, Scapin JP, Alarcón M. Infección respiratoria por Mycoplasma pneumoniae en pediatría. Arch Argent Pediatr. 2006; 104: 412-5.
13. Waites KB, Talkington D. Mycoplasma pneumoniae and its role as a human pathogen. Clin Microbiol Rev. 2004; 17: 697-728.
14. Higashigawa M, Kawasaki Y, Yodoya N, Omori Y, Nashida Y, Amemiya Y, et al. Prevalence of Mycoplasma IgM in children with lower respiratory tract illness. Pediatr Int. 2009; 51: 684-6.
15. Defilippi A, Silvestri M, Tacchella A, Giacchino R, Melioli G, Di Marco E, et al. Epidemiology and clinical features of Mycoplasma pneumoniae infection in children. Respir Med. 2008; 102: 1762-8.
16. Salas Mallea A. Infección por Mycoplasma pneumoniae en niños hospitalizados por neumonía. Rev Soc Bol Pediatr. 2007; 46: 163-70.
17. Hassan J, Irwin F, Dooley S, Connell J. Mycoplasma pneumoniae infection in a pediatric population: analysis of soluble immune markers as risk factors for asthma. Hum Immunol. 2008; 69: 851-5.
18. Atkinson TP, Balish MF, Waites KB. Epidemiology, clinical manifestations, pathogenesis and laboratory detection of Mycoplasma pneumoniae infections. FEMS Microbiol Rev. 2008; 32: 956-73.
19. Garnier JM, Noël G, Retornaz K, Blanc P, Minodier P. Extrapulmonary infections due to Mycoplasma pneumoniae. Arch Pediatr. 2005; 12 (Suppl 1): S2-6.
20. Othman N, Isaacs D, Daley AJ, Kesson AM. Mycoplasma pneumoniae infection in a clinical setting. Pediatr Int. 2008; 50: 662-6.
21. Dávila-Agüero G. Micoplasma en patología pulmonar pediátrica. Rev Peru Pediatr. 2007; 60: 101-4.
22. Mc Cracken GH. Diagnosis and management of pneumonia in children. Pediatr Infect Dis J. 2000; 19: 924-8.
23. Souliou E, Almasri M, Papa A, Theodoridou A. Diza E. Laboratory diagnosis of Mycoplasma pneumoniae respiratory tract infections in children. Eur J Clin Microbiol Infect Dis. 2007; 26: 513-5.
24. Loens K, Goossens H, Leven M. Acute respiratory infection due to Mycoplasma pneumoniae: current status of diagnostic method. Eur J Clin Microbiol Infect Dis. 2010; 29: 1055-69.
25. Sánchez-Ruiz-Cabello J, Maldonado-Espinosa MJ, Rubio-Quevedo C, Rosales-Zabel JM, Pereira-Rodríguez MJ, Holgado-Carballo MA. Neumonía por Mycoplasma pneumoniae en una zona básica de salud. An Esp Pediatr. 2001; 55: 108-12.