Iatrogenic bladder injury: A single institution's ten-year experience in treatment and outcome 1999-2009, Kuala Lumpur, Malaysia
Christopher CK Ho, MD1, Hans Alexander, MD2, Praveen Singam, MD1, Lee Boon Cheok, MD3, Zulkifli MD Zainuddin, MD4
1. Lecturer/Surgeon, Urology Unit, Department of Surgery, Universiti
Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia. e-mail: chrisckho2002@yahoo.com
2. Medical Officer, Urology Unit, Department of Surgery, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur, Malaysia.
3. Senior Lecturer/Consultant Urologist, Urology Unit, Department of
Surgery, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur,
Malaysia.
4. Associate Professor/Consultant Urologist, Urology Unit, Department of
Surgery, Universiti Kebangsaan Malaysia Medical Centre, Kuala Lumpur,
Malaysia.
Received for publication April 20, 2010 Accepted for publication October 19, 2010
SUMMARY
Introduction: This case series is a retrospective review of iatrogenic bladder injuries treated at our institution Universiti Kebangsaan Malaysia, Medical Centre, over a ten-year period, from 1999 to 2009.
Materials and methods: A retrospective review of the operating theater database yielded the names and registration numbers of patients who underwent operative repair of bladder injuries. Patients who sustained bladder injuries due to non-surgical reasons (such as traumatic bladder injuries due to pelvic fractures, blunt trauma or penetrating injuries to the pelvis) were excluded.
Results: There were 12 cases of iatrogenic bladder injury treated during this time. A total of eight injuries occurred during gynaecological surgery. Five injuries occurred during lower segment caesarean section, two injuries during total abdominal hysterectomy and bilateral salpingo-oopherectomy, and a single injury during Burch colposuspension. Four out of the five injuries during caesarian section had a history of previous caesarian section. Of the four remaining non-gynaecological related injuries, two injuries occurred during hernioplasty, one during exploration of an enterocutaneous fistula and the other was during laparoscopic appendicectomy.
Conclusion: Iatrogenic bladder injury should be anticipated in patients undergoing caesarean section who have had multiple previous caesarean sections. Iatrogenic injuries should be identified intra-operatively to enable early repair and the best outcome. These injuries were adequately assessed by ascending cystography. Continuous repair with absorbable sutures together with perivesicle drainage and bladder catheterization produces good outcome.
Keywords: Iatrogenic; Bladder; Injury; Repair.
Colomb Med. 2011; 42: 207-10
Lesión vesical iatrogénica: experiencia de diez años, tratamiento y resultados entre 1999-2009, Kuala Lumpur, Malasia
RESUMEN
Introducción: Esta serie del casos es una revisión retrospectiva de heridas iatrogénicas de vejiga tratadas en la Universidad Nacional de Malasia entre 1999 y 2009.
Métodos: Se hizo una revisión retrospectiva de la base de datos de la sala de cirugía del Centro Médico de la Universidad Nacional de Malasia, en individuos a quienes se les realizó cirugía de heridas de vejiga. Se excluyeron los pacientes que presentaron heridas de vejiga sin cirugía como heridas traumáticas debido a fracturas pélvicas, trauma cerrado o heridas penetrantes en la pelvis.
Resultados: Se encontraron 12 casos de herida de vejiga iatrogénica tratados entre 1999 y 2009. Ocho heridas ocurrieron durante cirugía ginecológica, 5 durante cesárea segmentaria baja, 2 durante histerectomía abdominal total y salpingo-ooforectomía bilateral y 1 herida durante colposuspensión de Burch. Las 4 heridas restantes no ginecológicas fueron: 2 heridas por iatrogenia ocurrida durante una hernioplastia, una durante exploración de una fístula entero-cutánea y la otra se presentó durante una apendectomía laparoscópica.
Conclusión: La herida iatrogénica de la vejiga debe ser anticipada en pacientes que experimentan cesárea que han tenido múltiples cesáreas previas. Las heridas iatrogénicas deben ser identificadas intra-operatoriamente para permitir reparación temprana y obtener el mejor resultado. Obtuvo mejores resultados la reparación continua con suturas absorbibles junto con drenaje vesical mediante catéter. La cistografía ascendente con 300 ml de contraste es la mejor opción para el diagnóstico de herida iatrogénica de vejiga y también para la evaluación de la reparación total.
Palabras clave: Iatrogenia; Vejiga; Herida; Reparación.
Colomb Med. 2011; 42: 207-10
Iatrogenic bladder injuries are an occasional complication of surgery performed in the pelvis. Anatomically, the bladder lies in close proximity to the rectum in men and to the uterus in women; thus there is potential for iatrogenic injury occurring during surgical dissection of the aforementioned structures. We present here our single institution's experience in dealing with iatrogenic bladder injury over a ten-year period.
MATERIALS AND METHODS
This is a retrospective review of all iatrogenic bladder injuries treated by our unit in our institution over the last ten years. The case notes were retrieved from the records office and the pertinent information was recorded onto a spreadsheet. Patients or their next of kin were contacted via phone to determine their current status if the patients were no longer on regular follow-up. Variables such as gender, age at the time of injury, and site of injury were recorded, as well as information about the indication for surgery, type of surgery performed, location of injury, when the injury was identified, method of repair and outcome of repair. Patients who sustained bladder injuries due to non-surgical reasons (such as traumatic bladder injuries due to pelvic fractures, blunt trauma or penetrating injuries to the pelvis) were excluded.
RESULTS
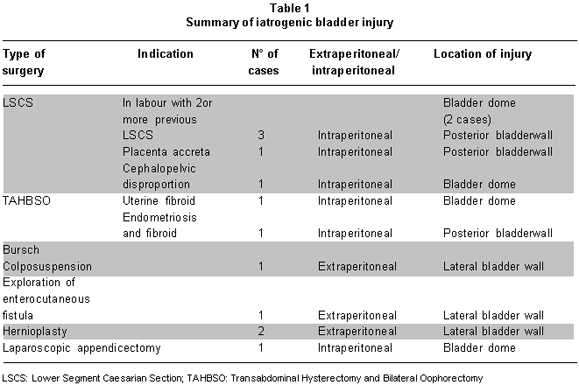
There were a total of 12 iatrogenic bladder injuries. Nine injuries occurred in female patients, while three injuries occurred in males. Table 1 shows the number of bladder injuries in relation to surgery performed, as well as the location of the injury. Eight injuries occurred during gynaecological surgery with five injuries occurring during lower segment caesarean section (LSCS), two injuries during total abdominal hysterectomy and bilateral salpingo-oopherectomy (TAHBSO), and one injury due to Burch colposuspension. Among the patients who sustained injury during caesarean section, four of these patients had previously undergone caesarean sections, while only one patient had no prior history of surgery.
Of the remaining four non-gynaecological surgery related injuries, two injuries occurred during open hernioplasty and one during exploration of an enterocutaneous fistula and the last during insertion of a suprapubic port for a laparoscopic appendicectomy. All injuries were referred to and repaired by the urology team upon diagnosis.
Eleven of the injuries were diagnosed intra-operatively. Only one case was diagnosed post-operatively via cystography after exploration of an enterocutaneous fistula. Post-operatively the patient was noted to have haematuria with rising serum creatinine levels with unilateral hydronephrosis on ultrasound. Cystography showed extraperitoneal extravasation of contrast, while retrograde pyelography showed a concurrent urethral injury causing the unilateral hydronephrosis. Repair of the bladder was performed together with repair of the urether, which was re-implanted by using a Boari flap.
Five injuries involved the dome of the bladder, three injuries occurred at the posterior wall, and four injuries occurred at the lateral wall of the bladder. Eight of the injuries were intraperitoneal, while the remaining four were extraperitoneal. All injuries were repaired primarily with absorbable sutures using the two-layer suture technique of the bladder wall with perivesical drainage.
Drainage of the bladder post repair was performed via a urethral catheter (Foley's catheter) for a minimum of ten days, which was removed only after cystography confirmed there was no urinary leak. Patients were then followed up with repeat retrograde cystography six months later and if normal, were discharged.
Ten patients were successfully treated with no complications and have remained well. One patient passed away due to unrelated causes. Another one, with a posterior wall intraperitoneal injury during LSCS, needed to be on catheter for three months due to persistent bladder leak. Her urine culture showed Escherichia coli infection, which was sensitive to cefuroxime. She was put on prolonged antibiotics. A repeat cystogram and urine culture at three months showed that the bladder had healed completely without any contrast extravasation and there was no more urinary infection. The catheter was removed and she has remained well at six months of follow up.
DISCUSSION
Bladder injury is a known complication of caesarean section and its incidence is reported at about 0.1 in 1000 births1. However, the risk is higher among patients who have undergone previous caesarean sections and present in labour necessitating emergency caesarean sections. Makoha et al.2, reported significantly higher risk of bladder injuries among patients with multiple caesarean sections due to the presence of intraperitoneal adhesions from previous surgery. Almost half of the iatrogenic bladder injuries in our series occurred during lower segment caesarean sections and all five caesarean sections were performed as emergencies. Furthermore, four of the five patients who sustained bladder injury during caesarean section had also previously undergone two or more caesarean sections prior to injury. Previous caesarean section is known to significantly increase the risk of iatrogenic bladder injury1-3.
Extraperitoneal injuries due to trauma can be safely treated non-surgically with just continuous bladder drainage4. Such injuries often result in retroperitoneal and scrotal urine extravasation but do not cause problems such as peritonitis, which is seen in intraperitoneal injuries. However, iatrogenic bladder injuries, which occur during surgery opens up a potential space for continued urine leak and fistula. All four extraperitoneal injuries in our series were surgically repaired as three injuries were detected intra-operatively, while the other was diagnosed later with a concurrent urethral injury requiring surgical intervention. The bladder injury repair was undertaken during reimplantation of the ureter. Despite the delayed diagnosis, the repair was a success with no complications two years later.
Surgical repair in this series utilized the continuous two-layered suturing method without difficulty. All patients, regardless of site of injury, were successfully repaired without any complications. All patients underwent cystography 10 days post repair and were followed up for at least 18 months before being discharged without further surveillance. In our experience, bladder repair is often successful with meticulous technique and proper debridement of the ragged wound edge to recreate a clean surgical wound edge for approximation and suturing.
Prompt diagnosis of iatrogenic injury and almost immediate repair in 11 out of 12 cases in this series is likely to have contributed to the good outcome seen in this series. It is well documented that early diagnosis and repair offers the best outcomes in the management of iatrogenic bladder injuries1,5. Delayed diagnosis often leads to the development of local infection, which usually progresses to sepsis; thereby, complicating repair, impairing wound healing, and producing poor outcomes.
Ascending cystography with a minimum of 300 ml of contrast insufflated into the bladder with two views followed by a post voiding film is adequate for the diagnosis of bladder injury and it provides all the anatomic details required for assessment and follow up. Ascending cystography was also advocated by Dobrowolski in his large series6. Continuous bladder drainage should be continued from repair until cystography confirms the integrity of the bladder repair. Perivesical drainage is recommended but should be removed after 48 hours post-operatively unless there is bleeding or extravasation of urine, which suggests an imperfect repair.
CONCLUSION
Prevention remains the best management of iatrogenic bladder injury. The risk of injury should be anticipated in patients undergoing emergency caesarean section who have prior history of multiple previous caesarean sections. Necessary precautions such as bladder decompression preoperatively and careful, meticulous dissection is important in reducing the risk. Of equal importance is for the surgeon to be alert and able to identify injury intra-operatively to facilitate immediate repair and achieve the best outcome.
Conflict of interest. None of the authors has conflicts of interest related to this study.
REFERENCES
1. Rajasekar D, Hall M. Urinary tract injuries during obstetric intervention. Br J Obstet Gynaecol. 1997; 104: 731-4.
2. Makoha FW, Felimban HM, Fathuddien MA, Roomi F, Ghabra T. Multiple cesarean section morbidity. Int J Gynaecol Obstet. 2004; 125: 50-3.
3. Rahman MS, Gasem T, Suleiman SA, Jama FEA, Burshaid S. Bladder injuries during caesarean section in a University Hospital: A 25-year review. Arch Gynecol Obstet. 2009; 279: 349-52.
4. Lynch TH, Martínez-Pineiro L, Plas Eugen, Serafetinides E, Turkeri L. EAU guidelines on urological trauma. Eur Urol. 2005; 47: 1-15.
5. Gómez RG, Ceballos L, Coburn M, Corriere JN, Dixon CM. Consensus on genitourinary trauma; Consensus statement on bladder injuries. Br J Urol. 2004; 94: 27-32.
6. Dobrowolski ZF, Lipczynski W, Drewniak T, Jakubik P, Kusionowicz J. External and iatrogenic trauma of urinary bladder: A survey in Poland. Br J Urol. 2002; 89: 755-6.