Case report: Multifocal chronic paracoccidioidomycosis in an adult
Karen Zapata, MD1, Janeth Villanueva, MD2, Adriana Arrunátegui, MD2, Juana Gabriela López, MD1
1. Dermatology Resident, Faculty of Health, School of Medicine, Universidad del Valle, Cali, Colombia. e-mail: kzuheyth@hotmail.com, juanalopez84@gmail.com
2. Dermatology Services Professor, Faculty of Health, School of Medicine, Universidad del Valle, Cali, Colombia. e-mail: janvirey@hotmail.com, adriana.arrunategui@imbanaco.com.co
Received for publication December 11, 2009 Accepted for publication August 17, 2010
SUMMARY
Paracoccidioides brasiliensis is the ethiological agent of one of the most prevalent systemic mycosis in Latin America, where around ten-million individuals are affected. Brazil has the highest incidence but in Venezuela, Colombia, Ecuador, and Argentina cases have also been reported. We describe a 56-year-old male with a one year history of lip, oral mucosa, and lung lesions. Granulomas and multinucleated giant cells were observed in histopathological evaluation with haematoxilyn-eosin stain. Mycologic studies (KOH and Gomori Grocott stain) showed blastoconidias with multiple budding. Serologic tests for paracoccidioidine were reactive. A diagnosis of chronic multifocal paracoccidioidomycosis was made. Initially, amphotericin B 0.7 mg/kg per day was started for fifteen days and consecutively itraconazole (400 mg/day) was administered orally with improvement of skin and lung lesions; however, an important residual fibrosis was observed. The patient was lost to follow up. We highlight the importance of an early diagnosis and adequate treatment to decrease sequelae in patient quality of life.
Keywords: Paracoccidioidomycosis; Paracoccidioides brasiliensis; Diagnosis, Amphotericin B; Itraconazole; Complications.
Colomb Med. 2011; 42: 228-32
Informe de caso: Paracoccidioidomicosis crónica multifocal del adulto
RESUMEN
Paracoccidioides brasiliensis es el agente causal de una de las micosis sistémicas con mayor prevalencia en Latinoamérica. Existen alrededor de 10 millones de afectados y la mayor incidencia se presenta en Brasil y se han observado casos en Venezuela, Colombia, Ecuador y Argentina. Se presenta el caso de un hombre de 56 años con lesiones de un año de evolución en labios, mucosa oral y pulmón. El estudio histopatológico con hematoxilina-eosina informó la presencia de granulomas y células gigantes multinucleadas. Los estudios micológicos (KOH y tinción de Gomori Grocott) mostraron blastoconidias con gemación múltiple. Las pruebas serológicas para paracoccidioidina fueron reactivas. Se diagnosticó un caso de paracoccidioidomicosis multifocal crónica y se inició tratamiento anfotericina B 0.7 mg/kg/día durante 15 días, luego itraconazol 400 mg diarios. Las lesiones cutáneas y pulmonares mejoraron; sin embargo, presentaba una fibrosis residual importante en la región oral y no continuó el seguimiento. Se resalta la importancia de realizar un diagnóstico temprano y disminuir las posibles secuelas que van a repercutir directamente sobre la calidad de vida del paciente.
Palabras clave: Paracoccidioidomicosis; Paracoccidioides brasiliensis; Diagnóstico; Anfotericina B; Itraconazol; Complicaciones.
Colomb Med. 2011; 42: 228-32
Paracoccidioidomycosis is a progressive, systemic mycosis caused by Paracoccidioides brasiliensis, a dimorphic fungus found in soils of some regions of Latin America; mainly between 30° latitude south and 34° latitude north1. The actual frequency is unknown because it is a not a disease of obligatory report.
CLINICAL CASE
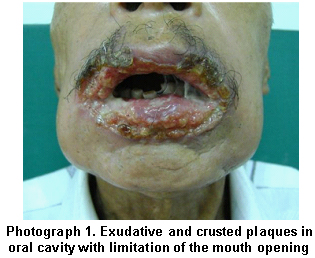
Herein, we present a case of a male patient, 56 years of age from the city of Pasto and residing in the city of Cali, Colombia; a street vendor, with a 10-month history since the apparition of papular lesions on the lips and gums. These lesions evolved into edemas, deformity, and ulcerated plaques with exudative crusts that compromised the whole oral cavity and were associated to weight loss, pain upon masticating and swallowing, limitation for opening the mouth and speaking. Then, verruciform plaques appeared on the second and fifth fingertips of the right hand and left hand, respectively, which progressed until revealing necrosis areas (Photographs 1, 2, and 3). The patient did not present other associated symptoms or relevant pathological antecedents.
The patient had an important epidemiological antecedent, he had emigrated from a wooded region, where he performed agricultural and carpentry tasks, to his current place of residence, an urban area located between coordinates 3°27'00''N and 76°32'00''W, geographically located on the Cauca River with a mean 1000-m altitude above sea level and a temperature of 25°C.
Complementary histopathological studies and laboratory studies were requested. Blood tests revealed homogeneous normochromic normocytic anemia, leukocytosis with neutrophilia, thrombocytosis, and the erythrocyte sedimentation rate of 50 mm/h. Renal function, hepatic function, and electrolytes did not show alterations. VDRL tests for syphilis and ELISA tests for HIV were negative, as well as the cutaneous tuberculin test, the Zielh-Neelsen stain for mycobacteria, and the Fite Faraco stain. A biopsy was performed of the lip lesions, which reported multiple-budding blastoconidia upon direct exam with potassium hydroxide at 20%. The histopathological study with hematoxylin-eosin reported epithelium with acantosis and abundant dermal inflammatory infiltrate with formation of granulomas and giant multinucleated cells. When staining with Gomori-Grocott, multiple budding blastoconidia were observed (Photograph 4).
The immunodiffusion test was also performed in agar gel with paracoccidioidine, reactive with one band of precipitate and the fixation of the complement, which was reactive to the 1:8 dilution. Thoracic X-ray revealed dense interstitial infiltrate with reticular zones in both pulmonary fields (Photograph 5).
Because of the cutaneous and pulmonary compromise, as well as of the oral mucosa, and confirmation through biopsy, the diagnosis indicated multifocal chronic paracoccidioidomycosis in an adult. Treatment was begun with amphotericin B 0.7 mg/kg/day (42 mg daily) for 15 days. Thereafter, treatment continued by administering itraconazole 200 mg every 12 hours for three months. This led to the patient presenting improvement of mucosa and pulmonary lesions; however, the patient presented marked limitation to open the mouth, secondary to fibrosis (Photograph 6). We requested plastic surgery and otolaryngology evaluation for its multidisciplinary management; nevertheless, the patient did not continue attending follow up controls and it has not been possible to continue assessing his therapeutical response or monitor existing sequelae.
DISCUSSION
Paracoccidioidomycosis is a chronic, granulomatous, systemic mycosis caused by the P. brasiliensis fungus2,3. Also called Lutz-Splendore-Almeida disease or South American blastomicosis, it was described by Adolfo Lutz in 1908 pseudococcidioidal granuloma; then in 1928, Almeida and Lacaz named the Paracoccidioides genus and in 1930, Almeida called the fungus Paracoccidioides brasiliensis1.
Thermal dimorphism is an important characteristic of the fungus, which is found as mold in nature between 4 and 25°C. Its rate of growth is relatively slow and it seems to present a restricted ability to compete or survive in the presence of the normal microbial flora of the soil4. A colony provided with short aerial mycelium was observed with hyaline septate hyphae, scarce microconidia , and chlamydoconidia. Between 35°C and 37°C, it grows as double-walled spherical yeast that reproduces by multiple budding, giving a «boat rudder» appearance5.
The habitat is still not well established; however, it has been isolated in tropical or subtropical regions with acid soils and temperatures varying between 17 and 24°C, in altitudes between sea level and 1500 meters, with a rainfall between 500 and 2500 mm/yearly. In these environments, the fungus exists as a plant and soil saprophyte2. The natural reservoir for P. brasiliensis is still under study, in recent years in several geographic regions of Brazil and Colombia species of infected armadillos have been described (Dasypus novemcinctus), before these discoveries it was considered that humans were its only host4.
In Latin America, there are close to 10-million individuals affected, but only 2% will develop the disease2. This systemic mycosis has a broad geographic distribution from Mexico to Argentina. Nevertheless, it does not occur in Nicaragua, Chile, or Guyana. The greatest incidence occurs in Brazil; cases have also been observed in Venezuela, Colombia, Ecuador, and Argentina2. The rate of incidence in Colombia between 1980 and 1999 was of 0.1 to 2.4 per 1'000,000 inhabitants, Antioquia, Santander, Cundinamarca, Meta, Caldas, Boyacá, and Tolima were identified as endemic departments -all are located in the country's central Eastern Andean region and the Magdalena River in Sierra Nevada of Santa Marta6. The distribution of paracoccidioidomycosis is heterogeneous in Colombia; in the case we are presenting, the patient was from the country's southwestern region, which is not within the endemic regions. But adequately diagnosing cases is important to be able to detect any change that may be presented in the region.
The rate of mortality in Brazil is of 1.45/1,000,000 inhabitants.7 It is most frequent in males with ratio of 10-15 to 1 with respect to females; in children an equal distribution is noted in both genders. Age ranges from childhood and adolescence to 30 to 50 years of age, where it may reach its greatest incidence; with 30 to 50 years being a productive age in life, thereby it bears a high social and economic impact. Although the entry route of the fungus is still a controversial issue, in most cases humans are mainly susceptible to infection by conidia inhalation.
The main risk factors for acquiring the disease involve activities related with the manipulation of contaminated soils or organic matter. Primo-infection usually occurs during the first decades of life with an incidence peak between 10 and 20 years of age, with the most frequent clinical manifestations between 30 and 50 years of age due to reactivation of a latent focus, which may develop, because of multiple factors that determine the immune status of the host like: age, use of immunosuppressive medications, and concomitant disease. The incubation period may last from some weeks to 60 years.
It is important to investigate the epidemiological antecedents, work activities, and migratory patterns because, for example, in our case the patient had performed agricultural tasks several years before in an area different to his domicile, which indicates that he probably acquired the infection from contaminated soils or organic matter, had a prolonged latency period, and migrated to a non-endemic area, which finally contributed to the presence of important sequelae.
There are several presentation forms from localized and benign to disseminated, severe and progressive, with important sequelae and poor prognosis. The clinical course may be acute or sub-acute in young individuals and chronic in adults. The most frequent classification used, established in the International Symposium on Paracoccidioidomycosis in Medellin, Colombia in 1986, is based on the clinical correlation and the disease's natural history and comprises: paracoccidioidomycosis infection, paracoccidioidomycosis disease, which includes acute/sub-acute form (juvenile type) that can be moderate or severe; chronic form (adult type) that can be unifocal (slight, moderate, and severe), multifocal (slight, moderate, and severe), and residual paracoccidioidomycosis8.
The acute/sub-acute form affects children, adolescents, and young adults; it is present in individuals up to 35 years of age, and has a short incubation period. The chronic form is the most frequent clinical presentation, usually affecting adult patients between 30 and 60 years of age. It is denominated unifocal when only one organ is affected, it generally affects more than one organ simultaneously (multifocal).
In 51 to 100% of the patients there is pulmonary affection with spotted bilateral infiltrate and hilar adenopathy; the progressive forms affect mostly the lower lobes and, in late stages, there is interstitial fibrosis. The oropharyngeal mucosa is affected in 51 to 82% of the cases, presenting increased volume, deformation, nodules and ulcerations that converge to form plaques1,2. These lesions may appear in the soft palate, gums, cheeks, floor of the mouth, tongue, and lips -constituting moriform stomatitis. Generally, the teeth become lose and some are lost; there is pain upon chewing and swallowing, which impedes ingestion and may lead to cachexia and death. Occasionally, there may be limitation to opening the mouth due to fibrosis. Because of the striking aspect of the central facial lesions, these have been denominated «tapir mouth». By extension, the pharynx, larynx, and trachea may be affected, even causing destruction of the epiglottis and the soft palate1,2.
The cutaneous areas affected tend to be the perioral and nasal regions; showing nodular and ulcerated, vegetative or verrucous, lesions of slow evolution and few symptoms. In case of nodal compromise, it is mainly noted in the cervical, inguinal, and supraclavicular regions.
Our patient presented pulmonary, cutaneous, and oropharyngeal mucosa compromise with a «tapir mouth» aspect, corresponding to a multifocal chronic case. The diagnosis was done by isolating and identifying the fungus via mycological exam through direct examination, culture, histopathology, and serological tests. Multiple budding with boat rudder aspect is pathognomonic of P. brasiliensis. The main culture media are Sabouraud agar and blood agar1,2,8.
The initial approach of patients with paracoccidioidomycosis constitutes a complete clinical evaluation with laboratory studies and X-rays to determine the degree of intensity and extension. The serological tests are diagnostic tools and help to evaluate the therapeutic response during follow up. This mycosis constitutes a diagnostic and therapeutic challenge because of the polymorphism of the lesions, chronicity, high costs, and lack of consensus on the treatment of choice, which include sulfonamides, amphotericin B, and imidazole derivatives like itraconazole and ketoconazole9.
We are presenting a case of multifocal chronic paracoccidioidomycosis in an adult, in an immunocompetent patient residing in an urban zone without apparent risk factors for acquiring the infection; however, with the antecedent of having resided in rural areas and performing agricultural tasks some years ago. The characteristics of our case highlight the importance of investigating the epidemiological antecedents in cases of polymorphous cutaneous manifestations to avoid delay in diagnosis and diminish possible sequelae that will impact directly on the patient's quality of life.
Conflict of interest. None of the authors has conflicts of interest related to this study.
REFERENCES
1. Arenas R. Micología médica ilustrada. 3ª ed. México, DF: Interamericana, McGraw-Hill; 2008.
2. Ramos e Silva M, Do Espirito Santo Saraiva L. Paracoccidioidomycosis. Dermatol Clin. 2008; 26: 257-69.
3. Poisson DM, Heitzmann A, Mille C, Muckensturm B, Dromer F, Dupont B, et al. Paracoccidioides brasiliensis in a brain abscess: first french case. J Mycol Med. 2007; 17: 114-8.
4. Bagagli E, Bosco S, Cordeiro R, Franco M. Phylogenetic and evolutionary aspects of Paracoccidioides brasiliensis reveal a long coexistence with animal host that explain several biological features of the pathogen. Infect Genet Evol. 2006; 6: 344-51.
5. Almeida AJ, Martins M, Carmona JA, Cano LE, Restrepo A, Leao C, et al. New insight into the cell cycle profile of Paracoccidioides brasiliensis. Fungal Genet Biol. 2006; 43: 401-9.
6. Torrado E, Castañeda E, De La Hoz F, Restrepo A. Paracoccidioidomicosis: definición de las áreas endémicas en Colombia. Biomedica. 2000; 20: 327-34.
7. Lyon A, Teixeira M, Araújo S, Pereira M, Pedroso E, Teixeira A. Serum levels of sTNF-R1, sTNF-R2 and CXCL9 correlate with disease activity in adult type paracoccidioidomycosis. Acta Trop. 2009; 109: 213-8.
8. Simao M. Paracoccidioidomycosis. Paediatr Respir Rev. 2009; 10: 161-5.
9. Menezes VM, Soares BGO, Fontes CJF. Drugs for treating paracoccydioidomycosis. Cochrane database of systematic reviews. 2006; 2. N° CD004967. DOI: 10.1002/14651858. CD004967.pub2.