Implementation of a new Single-Pass Whole-Body Computed Tomography Protocol: Is it safe, effective and efficient in patients with severe trauma?
Abstract
Purpose: The objective of this study was to evaluate the implementation of a new Single-Pass WBCT Protocol in the management of patients with severe trauma.
Methods: This was an observational, prospective study of polytrauma patients who underwent WBCT. Patients were divided into three groups: 1. Blunt trauma hemodynamically stable 2. Blunt trauma hemodynamically unstable and 3. Penetrating trauma. Demographics, WBCT parameters and outcome variables were evaluated.
Results: 263 patients were included. Median Injury Severity Score (ISS) was 22 (IQR: 16-22). Time between arrival to the ED and completing the WBCT was under 30 minutes in most patients [Group 1: 28 minutes (IQR: 14-55), Group 2: 29 minutes (IQR: 16-57), and Group 3: 31 minutes (IQR: 13-50); p=0.96]. 172 patients (65.4%) underwent non-operative management. The calculated and the real survival rates did not vary among the groups either [Group 1: TRISS 86.4% vs. RSR 85% (p=0.69); Group 2: TRISS 69% vs. RSR 74% (p=0.25); Group 3: TRISS 93% vs. RSR 87% (p=0.07)].
Conclusion: This new Single-Pass WBCT Protocol was safe, effective and efficient to decide whether the patient with severe trauma requires a surgical intervention independently of the mechanism of injury or the hemodynamic stability of the patient. Its use could also potentially reduce the rate of unnecessary surgical interventions of patients with severe trauma including those with penetrating trauma.
Authors
Downloads
Keywords
- Blunt and Penetrating Trauma
- Hemodynamic instability
- Whole-Body Computed Tomography
- Injury Severity Score
- Wounds, Nonpenetrating
- Abdominal Injuries
- Emergency Service
- Decision Making
- Tomography, X-Ray Computed* / mortality
- Tomography, X-Ray Computed* / statistics & numerical data
- Whole Body Imaging* / mortality
- Whole Body Imaging* / statistics & numerical data
- Wounds, Nonpenetrating / diagnostic imaging
References
Chidambaram S, Goh EL, Khan MA. A meta-analysis of the efficacy of whole-body computed tomography imaging in the management of trauma and injury. Injury. 2017;48(8):1784-1793.https://doi.org/10.1016/j.injury.2017.06.003 PMid:28610777
ATLS Subcommittee. American College of Surgeons' Committee on Trauma. International ATLS working group Advanced trauma life support (ATLS) J Trauma Acute Care Surg. 2013;74(5):1363-1366. https://doi.org/10.1097/TA.0b013e31828b82f5 PMid:23609291
Soto JA, Anderson SW. Multidetector CT of Blunt Abdominal Trauma. Radiology. 2012;265(3):678-693. https://doi.org/10.1148/radiol.12120354 PMid:23175542
Wada D, Nakamori Y, Yamakawa K, Yoshikawa Y, Kiguchi T, Tasaki O. Impact on survival of whole-body computed tomography before emergency bleeding control in patients with severe blunt trauma. Crit Care. 2013;17(4):R178-R178. https://doi.org/10.1186/cc12861 PMid:24025196 PMCid:PMC4057394
Hoffstetter P, Herold T, Daneschnejad M, Zorger N, Jung E, Feuerbach S. Non-trauma-associated additional findings in whole-body CT examinations in patients with multiple trauma. Rofo. 2008;180(2):120-126. https://doi.org/10.1055/s-2007-963594 PMid:18008192
Dreizin D, Munera F. Multidetector CT for Penetrating Torso Trauma State of the Art. Radiology. 2015;277(2):338-355. https://doi.org/10.1148/radiol.2015142282 PMid:26492022
Huber-Wagner S, Lefering R, Qvick LM, Körner M, Kay MV, Pfeifer KJ. Effect of whole-body CT during trauma resuscitation on survival a retrospective, multicentre study. Lancet. 2009;373(9673):1455-1461. https://doi.org/10.1016/S0140-6736(09)60232-4
Tsutsumi Y, Fukuma S, Tsuchiya A, Yamamoto Y, Fukuhara S. Whole-Body Computed Tomography During Initial Management and Mortality Among Adult Severe Blunt Trauma Patients A Nationwide Cohort Study. World J Surg. 2018;42(12):3936-3946. https://doi.org/10.1007/s00268-018-4732-5 PMid:29959493
Kinoshita T, Yamakawa K, Matsuda H, Yoshikawa Y, Wada D, Hamasaki T. The Survival Benefit of a Novel Trauma Workflow that Includes Immediate Whole-body Computed Tomography, Surgery, and Interventional Radiology, All in One Trauma Resuscitation Room A Retrospective Historical Control Study. Ann Surg. 2019;269(2):370-376. https://doi.org/10.1097/SLA.0000000000002527 PMid:28953551 PMCid:PMC6325752
Hutter M, Woltmann A, Hierholzer C, Gärtner C, Bühren V, Stengel D. Association between a single-pass whole-body computed tomography policy and survival after blunt major trauma A retrospective cohort study. Scand J Trauma Resusc Emerg Med. 2011;19(1):73-73. https://doi.org/10.1186/1757-7241-19-73 PMid:22152001 PMCid:PMC3267654
Huber-Wagner S, Lefering R, Qvick L-M, Körner M, Kay M V, Pfeifer K-J K-J. Effect of whole-body CT during trauma resuscitation on survival a retrospective, multicentre study. Lancet. 2009;373(9673):1455-1461. https://doi.org/10.1016/S0140-6736(09)60232-4
Kimura A, Tanaka N. Whole-body computed tomography is associated with decreased mortality in blunt trauma patients with moderate-to-severe consciousness disturbance. J Trauma Acute Care Surg. 2013;75(2):202-206. https://doi.org/10.1097/TA.0b013e3182905ef7 PMid:23702629
Jiang L, Ma Y, Jiang S, Ye L, Zheng Z, Xu Y. Comparison of whole-body computed tomography vs selective radiological imaging on outcomes in major trauma patients a meta-analysis. Scand J Trauma Resusc Emerg Med. 2014;22(1):54-54. https://doi.org/10.1186/s13049-014-0054-2 PMid:25178942 PMCid:PMC4347587
Smith C, Woolrich-Burt L, Wellings R, Costa M. Major trauma CT scanning the experience of a regional trauma centre in the UK. Emerg Med L. 2011;28(5):378-382. https://doi.org/10.1136/emj.2009.076414 PMid:20515906
Huber-Wagner S, Biberthaler P, Häberle S, Wierer M, Dobritz M, Rummeny E. Whole-Body CT in Haemodynamically Unstable Severely Injured Patients - A Retrospective, Multicentre Study. PLoS One. 2013;8(7):e68880. https://doi.org/10.1371/journal.pone.0068880 PMid:23894365 PMCid:PMC3722202
Committee on Trauma. American College of Surgeons . Advanced Trauma Life Support for Doctors - Student Course Manual. Committee on Trauma, American College of Surgeons; Chicago: 2008.
Hakim W, Kamanahalli R, Dick E, Bharwani N, Fetherston S, Kashef E. Trauma whole-body MDCT An assessment of image quality in conventional dual-phase and modified biphasic injection. Br J Radiol. 2016;89:20160160-20160160. https://doi.org/10.1259/bjr.20160160 PMid:27187601 PMCid:PMC5257328
Stengel D, Frank M, Matthes G, Schmucker U, Seifert J, Mutze S. Primary pan-computed tomography for blunt multiple trauma can the whole be better than its parts? Injury. 2009;40(Suppl 4):36-46. https://doi.org/10.1016/j.injury.2009.10.035 PMid:19895951
Brenner D, Elliston C. Estimated Radiation Risks Potentially Associated with Full-Body CT Screening. Radiology. 2004;232(3) https://doi.org/10.1148/radiol.2323031095 PMid:15273333
Brenner DJ, Hall EJ. Computed Tomography - An Increasing Source of Radiation Exposure. N Engl J Med. 2007;357(22):2277-2284. https://doi.org/10.1056/NEJMra072149 PMid:18046031
Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours A retrospective cohort study. Lancet. 2012;380(9840):499-505.https://doi.org/10.1016/S0140-6736(12)60815-0
Hickethier T, Mammadov K, Baeßler B, Lichtenstein T, Hinkelbein J, Smith L. Whole-body computed tomography in trauma patients Optimization of the patient scanning position significantly shortens examination time while maintaining diagnostic image quality. Ther Clin Risk Manag. 2018;14:849-859. https://doi.org/10.2147/TCRM.S162074 PMid:29765226 PMCid:PMC5944460
Boscak AR, Shanmuganathan K, Mirvis SE, Fleiter TR, Miller LA, Sliker CW. Optimizing Trauma Multidetector CT Protocol for Blunt Splenic Injury Need for Arterial and Portal Venous Phase Scans. Radiology. 2013;268(1):79-88. https://doi.org/10.1148/radiol.13121370 PMid:23449955
Scialpi M, Schiavone R. Single-pass split-bolus CT protocol in polytrauma Reproducibility and diagnostic efficacy. Acta Radiol. 2015;56(12):NP47-NP48. https://doi.org/10.1177/0284185115610936 PMid:26582938
Nguyen D, Platon A, Shanmuganathan K, Mirvis S, Becker C, Poletti P. Evaluation of a single-pass continuous whole-body 16-MDCT protocol for patients with polytrauma. AJR Am J Roentgenol. 2009;192(1):3-10. https://doi.org/10.2214/AJR.07.3702 PMid:19098172
Geyer LL, Körner M, Harrieder A, Mueck FG, Deak Z, Wirth S. Dose reduction in 64-row whole-body CT in multiple trauma An optimized CT protocol with iterative image reconstruction on a gemstone-based scintillator. Br J Radiol. 2016;89(1061):e20160003. https://doi.org/10.1259/bjr.20160003 PMid:26853510 PMCid:PMC4985483
Iacobellis F, Scaglione M, Ierardi AM, Carrafiello G, Mazzei MA, Biasina AM. Dual-phase CT for the assessment of acute vascular injuries in high-energy blunt trauma The imaging findings and management implications. Br J Radiol. 2016;89(1061):20150952-20150952. https://doi.org/10.1259/bjr.20150952 PMid:26882960 PMCid:PMC4985472
Brenner DJ, Elliston CD. Estimated Radiation Risks Potentially Associated with Full-Body CT Screening. Radiology. 2004;232(3):735-738. https://doi.org/10.1148/radiol.2323031095 PMid:15273333
Sierink JC, Treskes K, Edwards MJR, Beuker BJA, den Hartog D, Hohmann J. Immediate total-body CT scanning versus conventional imaging and selective CT scanning in patients with severe trauma (REACT-2) a randomised controlled trial. Lancet. 2016;388(10045):673-683. https://doi.org/10.1016/S0140-6736(16)30932-1
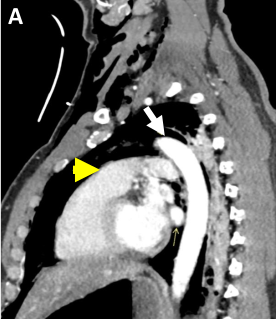
Ordoñez CA, Herrera-Escobar JP, Parra MW. Computed Tomography in Hemodynamically Unstable Severely Injured Blunt and Penetrating Trauma Patients. J Trauma Acute Care Surg. 2016;80(4):597-602. https://doi.org/10.1097/TA.0000000000000975 PMid:26808032
Copyright (c) 2020 Universidad del Valle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-4495-7405
https://orcid.org/0000-0003-4495-7405


















