Damage control in penetrating duodenal trauma: less is better
Abstract
The overall incidence of duodenal injuries in severely injured trauma patients is between 0.2 to 0.6% and the overall prevalence in those suffering from abdominal trauma is 3 to 5%. Approximately 80% of these cases are secondary to penetrating trauma which are commonly associated with vascular and adjacent organ injuries. Therefore, defining the best surgical treatment algorithm remains controversial. Mild to moderate duodenal trauma is currently managed via primary repair and simple surgical techniques. However, severe injuries have required complex surgical techniques without significant favorable outcomes and consequential increase in the rates of mortality. The aim of this article is to delineate the experience in the surgical management of penetrating duodenal injuries via the creation of a practical and effective algorithm that includes basic principles of damage control surgery which sticks to the philosophy of “Less is Better”. Surgical management of all penetrating duodenal trauma should always default when possible to primary repair. When confronted with a complex duodenal injury, hemodynamic instability and/or significant associated injuries then the default should be damage control surgery. Definitive reconstructive surgery should be postponed until the patient has been adequately resuscitated and the diamond of death has been corrected.
Authors
Downloads
Keywords
- Penetrating duodenal trauma
- primary repair
- duodenal reconstruction
- primary anastomosis
- damage control surgery
- Injury Severity Score
- Trauma Centers
- Laparotomy
- Retropneumoperitoneum
- Pancreaticoduodenectomy
- Jejunostomy
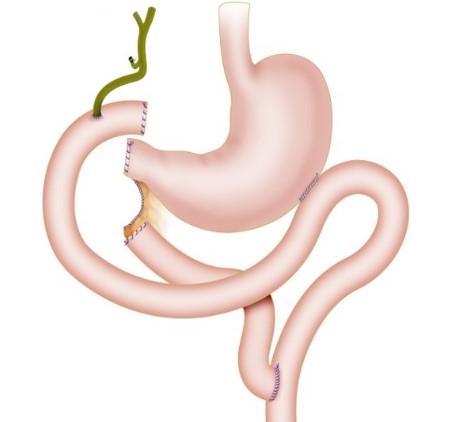
- Gastric Bypass
- Duodenum
- Balloon Occlusion
References
Asensio J, Feliciano D, Britt L, Kerstein M. Management of duodenal injuries. Trauma 2012;14:3–15. https://doi.org/10.1177/1460408611412316.
Rickard MJFX, Brohi K, Bautz PC. Pancreatic and duodenal injuries: Keep it simple. ANZ J Surg 2005;75:581–6. https://doi.org/10.1111/j.1445-2197.2005.03351.x.
Hong J, Wang SY, Qian L, Chen Z you. Diagnosis and Treatment of Duodenal Injury: A Clinical Analysis. Hepatogastroenterology 2015;62:641–6.
Ordoñez C, García A, Parra MW, Scavo D, Pino LF, Millán M, et al. Complex penetrating duodenal injuries: Less is better. J Trauma Acute Care Surg 2014;76:1177–83. https://doi.org/10.1097/TA.0000000000000214.
Leppäniemi A. Focus on pancreatic and duodenal injuries. Eur J Trauma Emerg Surg 2007;33:219–20. https://doi.org/10.1007/s00068-007-2004-4.
Talving P, Nicol AJ, Navsaria PH. Civilian duodenal gunshot wounds: Surgical management made simpler. World J Surg 2006;30:488–94. https://doi.org/10.1007/s00268-005-0245-0.
Girgin S, Gedik E, Yaǧmur Y, Uysal E, Baç B. Management of duodenal injury: Our experience and the value of tube duodenostomy. Ulus Travma ve Acil Cerrahi Derg 2009;15:467–72.
Feliciano D. Abdominal Trauma Revisited. Am Surg 2017;83.
Ivatury RR, Nallathambi M, Gaudino J, Rohman M, Stahl WM. Penetrating duodenal injuries. Analysis of 100 consecutive cases. Ann Surg 1985;202:153–8. https://doi.org/10.1097/00000658-198508000-00003.
Schroeppel TJ, Saleem K, Sharpe JP, Magnotti LJ, Jordan AW, Fischer PE, et al. Penetrating duodenal trauma: A 19-year experience. J Trauma Acute Care Surg 2016;80:461–5. https://doi.org/10.1097/TA.0000000000000934.
Aiolfi A, Matsushima K, Chang G, Bardes J, Strumwasser A, Lam L, et al. Surgical Trends in the Management of Duodenal Injury. J Gastrointest Surg 2019;23:264–9. https://doi.org/10.1007/s11605-018-3964-x.
Advanced trauma life support (ATLS): 10th Edition. 2018. https://doi.org/10.1111/j.1365-2044.1993.tb07026.x.
Coccolini F, Kobayashi L, Kluger Y, Moore EE, Ansaloni L, Biffl W, et al. Duodeno-pancreatic and extrahepatic biliary tree trauma: WSES-AAST guidelines. World J Emerg Surg 2019;14. https://doi.org/10.1186/s13017-019-0278-6.
Ordoñez CA, Herrera-Escobar JP, Parra MW, Rodriguez-Ossa PA, Mejia DA, Sanchez AI, et al. Computed tomography in hemodynamically unstable severely injured blunt and penetrating trauma patients. J Trauma Acute Care Surg 2016;80:597–603. https://doi.org/10.1097/TA.0000000000000975.
Choi AY, Bodanapally UK, Shapiro B, Patlas MN, Katz DS. Recent Advances in Abdominal Trauma Computed Tomography. Semin Roentgenol 2018;53:178–86. https://doi.org/10.1053/j.ro.2018.02.008.
Joseph DK, Kunac A, Kinler RL, Staff I, Butler KL. Diagnosing blunt hollow viscus injury: Is computed tomography the answer? Am J Surg 2013;205:414–8. https://doi.org/10.1016/j.amjsurg.2012.12.003.
Osborn LA, Brenner ML, Prater SJ, Moore LJ. Resuscitative endovascular balloon occlusion of the aorta: Current evidence. Open Access Emerg Med 2019;11:29–38. https://doi.org/10.2147/OAEM.S166087.
Slavini J, Ghaneh P, Sutton R, Hartley M, Rowlands P, Garvey C, et al. management of necrotizing pancreatitis. Gastroenterology 1989;97:510–1. https://doi.org/10.1016/0016-5085(89)90097-8.
Fang JF, Chen RJ, Lin BC, Hsu YB, Kao JL, Kao YC, et al. Retroperitoneal laparostomy: An effective treatment of extensive intractable retroperitoneal abscess after blunt duodenal trauma. J Trauma - Inj Infect Crit Care 1999;46:652–5. https://doi.org/10.1097/00005373-199904000-00015.
Doglietto GB, Pacelli F, Caprino P, Alfieri S, Tortorelli AP, Mutignani M. Posterior laparostomy through the bed of the 12th rib to drain retroperitoneal infection after endoscopic sphincterotomy. Br J Surg 2004;91:730–3. https://doi.org/10.1002/bjs.4544.
Doglietto GB, Prete Pacelli Prete F, Papa V, Tortorelli AP, F. R. Posterior laparostomy for retroperitoneal infections caused by periampullar endoscopic procedures: an old technique for an emerging disease. Chir Ital 2004;56:163–8.
Phillips B, Turco L, McDonald D, Mause A, Walters RW. Penetrating injuries to the duodenum: An analysis of 879 patients from the National Trauma Data Bank, 2010 to 2014. J Trauma Acute Care Surg 2017;83:810–7. https://doi.org/10.1097/TA.0000000000001604.
Ferrada P, Wolfe L, Duchesne J, Fraga GP, Benjamin E, Alvarez A, et al. management of duodenal trauma: A retrospective review from the Panamerican Trauma Society. J Trauma Acute Care Surg 2019;86:392–6. https://doi.org/10.1097/TA.0000000000002157.
Moore E, Cogbill T, Malangoni M, Jurkovich G, Champion H, Gennarelli T, et al. Organ injury scaling, II: pancreas, duodenum, small bowel, colon and rectum. J Trauma 1990;30:1427–9.
Copyright (c) 2021 Universidad del Valle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-4495-7405
https://orcid.org/0000-0003-4495-7405


















