Drug-induced liver injury after covid-19 mRNA vaccine: case report
Abstract
Case description:
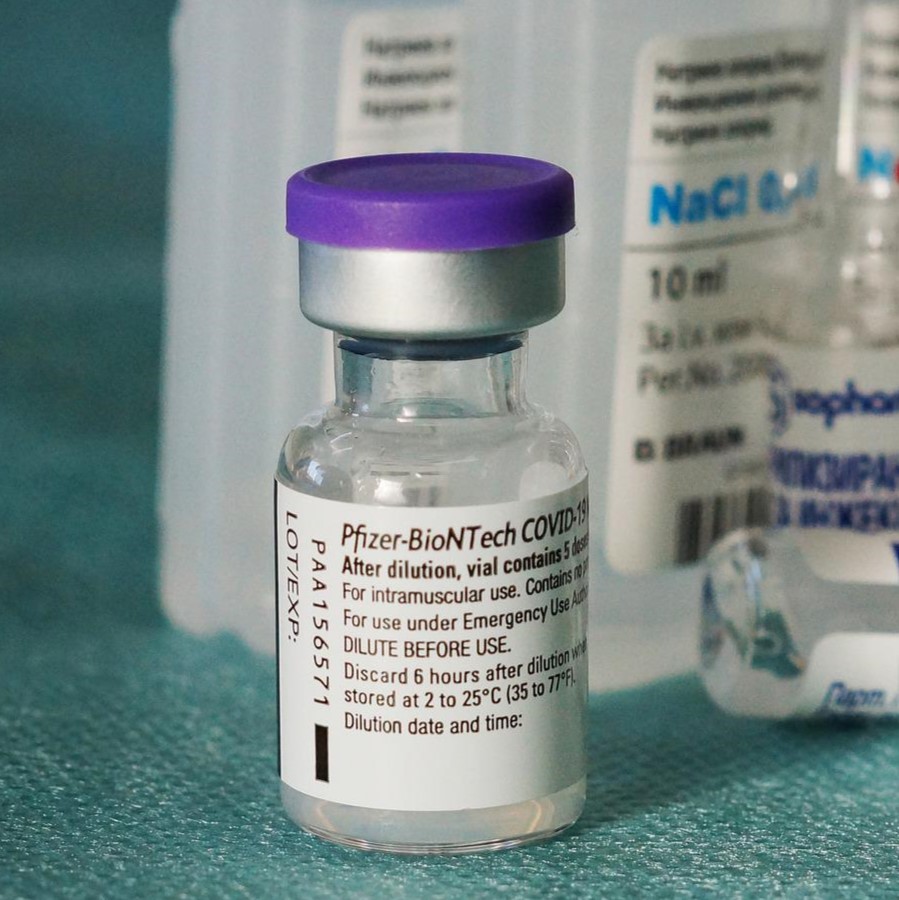
A 22-year-old female patient received the first dose of Pfizer-BioNTech vaccine (RNAm) against COVID-19; 6 days later, she presented abdominal pain located in the right hypochondrium and epigastrium, associated with emetic episodes. Consultation 21 days later due to the same symptoms; three days after the second
dose of the vaccine was administered.
Clinical findings:
Pain on palpation in the right hypochondrium. Laboratories reported hepatocellular lesions and cholestasis, with negative amylase, hepatotropic virus and autoimmune hepatitis tests. Liver and biliary tract ultrasound and cholangioresonance were normal.
Treatment and Results:
Hyoscine and intravenous fluids as support therapy. She presented improvement in abdominal pain and a progressive decrease of transaminases and bilirubin levels until normalization and was discharged on the fifth day of hospitalization. A drug-associated hepatotoxicity (DILI) diagnosis was considered probable, in this case, secondary to vaccination against COVID-19.
Clinical Relevance:
The current SARS-CoV-2 pandemic has spurred the development of new vaccines, the safety of which remains a concern. There is a likely causal relationship between vaccination and liver involvement in this clinical case rather than simply a sporadic occurrence.
Authors
Downloads
Keywords
- COVID-19
- mRNA vaccine
- Autoimmune hepatitis
- Hepatotoxicity
- Chemical and drug induced liver injury
- Liver function tests
- Pharmacovigilance
- Adverse vaccine reaction
References
IHR. Emergency Committee on Novel Coronavirus (2019-nCoV). 25 de enero de 2021. Disponible en https://www.who.int/dg/speeches/detail/who-director-general-s-statement-on-ihr-emergencycommittee- on-novel-coronavirus-(2019-ncov). https://doi.org/10.2807/1560-7917.ES.2020.25.3.2001231
Bril F, Al Diffalha S, Dean M, Fettig DM. Autoimmune hepatitis developing after coronavirus disease 2019 (COVID-19) vaccine: Causality or casualty? J Hepatol. 2021; 75:222-224. https://doi.org/10.1016/j.jhep.2021.04.003 PMid:33862041 PMCid:PMC8056822
Mulligan MJ, Lyke KE, Kitchin N, et al. Phase I/II study of COVID-19 RNA vaccine BNT162b1 in adults. Nature [Internet]. 2020;586(7830):589-593. Disponible en: doi: 10.1038/s41586-020-2639-4. https://doi.org/10.1038/s41586-020-2639-4 PMid:32785213
Rocco A, Sgamato C, Compare D, Nardone G. Autoimmune hepatitis following SARS-CoV-2 vaccine: May not be a casualty. J Hepatol. 2021. https://doi.org/10.1016/j.jhep.2021.05.038 PMid:34116081 PMCid:PMC8186938
Tan CK, Wong YJ, Wang LM, Ang TL, Kumar R. Autoimmune hepatitis following COVID-19 Vaccination: true causality or mere association? J Hepatol. 2021. https://doi.org/10.1016/j.jhep.2021.06.009 PMid:34153398 PMCid:PMC8404983
McShane C, Kiat C, Rigby J, Crosbie O. The mRNA COVID-19 vaccine - a rare trigger of Autoimmune Hepatitis? J Hepatol. 2021. https://doi.org/10.1016/j.jhep.2021.06.044 PMid:34245804 PMCid:PMC8264276
Zhou T, Fronhoffs F, Dold L, Strassburg CP, Weismüller TJ. New-Onset Autoimmune Hepatitis following mRNA Covid-19 Vaccination in a 36- year-old woman with Primary Sclerosing Cholangitis - should we be more vigilant? J Hepatol [Internet]. 2022;76(1):218-220. Disponible en: doi: 10.1016/j.jhep.2021.08.006. https://doi.org/10.1016/j.jhep.2021.08.006 PMid:34450237 PMCid:PMC8384483
Jothimani D, Venugopal R, Abedin MF, Kaliamoorthy I, Rela M. COVID-19 and the liver. J Hepatol. 2020; 73:1231-40.https://doi.org/10.1016/j.jhep.2020.06.006 PMid:32553666 PMCid:PMC7295524
Kwo, P. Y., Cohen, S. M., & Lim, J. K. ACG clinical guideline: Evaluation of abnormal liver chemistries. The American Journal of Gastroenterology. 2017;112(1):18-35. https://doi.org/10.1038/ajg.2016.517. PMid:27995906
World Health Organization. Safety of medicines: a guide to detecting and reporting adverse drug reaction. Geneva: WHO. 2002.
Naranjo, C. A., Busto, U., Sellers, E. et al. A method for estimating the probability of adverse drug reactions. Clinical Pharmacology and Therapeutics. 1981;30(2):239-245. https://doi.org/10.1038/clpt.1981.154. PMid:7249508
Polack, F. P., Thomas, S. J., Kitchin, N., et al. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. The New England Journal of Medicine, 2020;383(27):2603-2615. https://doi.org/10.1056/NEJMoa2034577. PMid:33301246 PMCid:PMC7745181
Falsey, A. R., Sobieszczyk, M. E., Hirsch, I., et al. Phase 3 safety and efficacy of AZD1222 (ChAdOx1 nCoV-19) Covid-19 vaccine. The New England Journal of Medicine, 2021;385(25):2348-2360. https://doi.org/10.1056/NEJMoa2105290. PMid:34587382 PMCid:PMC8522798
Tanriover, M. D., Doğanay, H. L., Akova, M., et al. Efficacy and safety of an inactivated whole-virion SARS-CoV-2 vaccine (CoronaVac): interim results of a double-blind, randomized, placebo-controlled, phase 3 trial in Turkey. Lancet. 2021;398(10296): 213-222. https://doi.org/10.1016/S0140-6736(21)01429-X.
El Sahly, H. M., Baden, L. R., Essink, B., Doblecki-Lewis, S., Martin, J. M., Anderson, E. J., Campbell, T. B., Clark, J., Jackson, L. A., Fichtenbaum, C. J., Zervos, M., Rankin, B., Eder, F., Feldman, G., Kennelly, C., Han-Conrad, L., Levin, M., Neuzil, K. M., Corey, L., COVE Study Group. (2021). Efficacy of the mRNA-1273 SARS-CoV-2 vaccine at completion of blinded phase. The New England Journal of Medicine, 385(19), 1774-1785. https://doi.org/10.1056/NEJMoa2113017. PMid:34551225 PMCid:PMC8482810
Print C-mPBva: All UK Spontaneous Reports Received Between 9/12/20 and 26/05/21 for mRNA Pfizer/BioNTech Vaccine Analysis Print. 2021.
Shroff, H., Satapathy, S. K., Crawford, J. M., Todd, N. J., & VanWagner, L. B. Liver injury following SARS-CoV-2 vaccination: A multicenter case series. J Hepatol. 2022;76(1): 211-214. https://doi.org/10.1016/j.jhep.2021.07.024. PMid:34339763 PMCid:PMC8324396
Alqarni M M, Faloudah A Z, Alsulaihebi A S, et al. A Case of Hepatotoxicity After Receiving a COVID-19 Vaccine. Cureus [Internet]. 2021;13(12): e20455. https://doi.org/10.7759/cureus.20455
Mann R, Sekhon S, Sekhon S. Drug-induced liver injury after COVID-19 vaccine. Cureus [Internet]. 2021;13: e16491 https://doi.org/10.7759/cureus.16491
Kleiner, D. E. Drug-induced liver injury: The hepatic pathologist's approach. Gastroenterol Clin North Am.2017;46(2),273-296. https://doi.org/10.1016/j.gtc.2017.01.004. PMid:28506365 PMCid:PMC5434713
Morales Maya, L., Vélez López, N., & Muñoz Maya, O. Hepatotoxicidad: patrón colestásico inducido por fármacos. Rev Colomb Gastroenterol. 2016;31(1),36. https://doi.org/10.22516/25007440.71.
Danan, G., & Teschke, R. RUCAM in drug and herb induced liver injury: The update. Int J Mol Sci. 2015;17(1),14. https://doi.org/10.3390/ijms17010014. PMid:26712744 PMCid:PMC4730261
Hoofnagle, J. H., & Björnsson, E. S. Drug-induced liver injury-types and phenotypes. The New England Journal of Medicine. 2015;381(3),264-273. https://doi.org/10.1056/NEJMra1816149. PMid:31314970
Copyright (c) 2022 Universidad del Valle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-1061-309X
https://orcid.org/0000-0003-1061-309X


















