Pancreatic Damage Control: The Pancreas is Simple Don’t Complicate It
Abstract
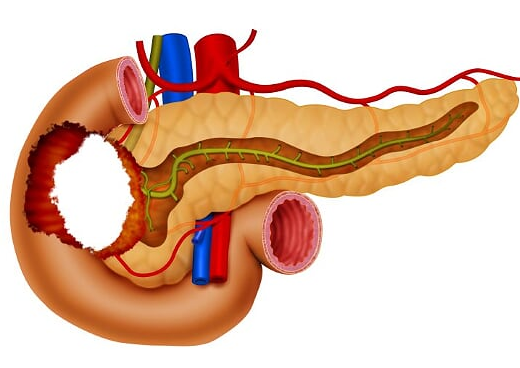
Pancreatic trauma is a rare but potentially lethal injury because often it is associated with other abdominal organ or vascular injuries. Usually, it has a late clinical presentation which in turn complicates the management and overall prognosis. Due to the overall low prevalence of pancreatic injuries, there has been a significant lack of consensus among trauma surgeons worldwide on how to appropriately and efficiently diagnose and manage them. The accurate diagnosis of these injuries is difficult due to its anatomical location and the fact that signs of pancreatic damage are usually of delayed presentation. The current surgical trend has been moving towards organ preservation in order to avoid complications secondary to exocrine and endocrine function loss and/or potential implicit post-operative complications including leaks and fistulas. The aim of this paper is to propose a management algorithm of patients with pancreatic injuries via an expert consensus. Most pancreatic injuries can be managed with a combination of hemostatic maneuvers, pancreatic packing, parenchymal wound suturing, and closed surgical drainage. Distal pancreatectomies with the inevitable loss of significant amounts of healthy pancreatic tissue must be avoided. General principles of damage control surgery must be applied when necessary followed by definitive surgical management when and only when appropriate physiological stabilization has been achieved. It is our experience that viable un-injured pancreatic tissue should be left alone when possible in all types of pancreatic injuries accompanied by adequate closed surgical drainage with the aim of preserving primary organ function and decreasing short and long-term morbidity.
Authors
Downloads
Keywords
- Pancreatic Damage Control
- Suture
- Drainage
- Pancreatic Fistula
- Pancreatectomy
- Peritoneal Cavity
- Amylases
- Ampulla of Vater
- Enteral Nutrition
- Splenectomy
- Negative-Pressure Wound Therapy
- Critical Illness
- Cholecystostomy
- Operating Rooms
- Laparotomy
- Lacerations
References
Iacono C, Zicari M, Conci S, Valdegamberi A, De Angelis M, Pedrazzani C, et al. Management of pancreatic trauma: A pancreatic surgeon's point of view. Pancreatology 2016;16:302-8. https://doi.org/10.1016/j.pan.2015.12.004
Wiik Larsen J, Søreide K. The worldwide variation in epidemiology of pancreatic injuries. Injury 2019;50:1787-9. https://doi.org/10.1016/j.injury.2019.08.010
Coccolini F, Kobayashi L, Kluger Y, Moore EE, Ansaloni L, Biffl W, et al. Duodeno-pancreatic and extrahepatic biliary tree trauma: WSES-AAST guidelines. World J Emerg Surg 2019;14. https://doi.org/10.1186/s13017-019-0278-6
Ahmed N, Vernick JJ. Pancreatic injury. South Med J 2009;102:1253-6. https://doi.org/10.1097/SMJ.0b013e3181c0dfca
Vasquez M, Cardarelli C, Glaser J, Murthi S, Stein D, Scalea T. The ABC's of Pancreatic Trauma: Airway, Breathing, and Computerized Tomography Scan? Mil Med 2017;182:66-71. https://doi.org/10.7205/milmed-d-16-00084
Krige JEJ, Kotze UK, Setshedi M, Nicol AJ, Navsaria PH. Management of pancreatic injuries during damage control surgery: an observational outcomes analysis of 79 patients treated at an academic Level 1 trauma centre. Eur J Trauma Emerg Surg 2017;43:411-20. https://doi.org/10.1007/s00068-016-0657-6
Petrone P, Moral Álvarez S, González Pérez M, Ceballos Esparragón J, Marini CP. Traumatismos de páncreas: manejo y revisión de la literatura. Cir Esp 2017;95:123-30. https://doi.org/10.1016/j.ciresp.2016.05.011
Jurkovich GJ. Pancreatic trauma. J Trauma Acute Care Surg 2020;88:19-24. https://doi.org/10.1097/TA.0000000000002546
Sharpe JP, Magnotti LJ, Weinberg JA, Zarzaur BL, Stickley SM, Scott SE, et al. Impact of a defined management algorithm on outcome after traumatic pancreatic injury. J. Trauma Acute Care Surg., vol. 72, J Trauma Acute Care Surg; 2012, p. 100-5. https://doi.org/10.1097/TA.0b013e318241f09d
Shibahashi K, Sugiyama K, Kuwahara Y, Ishida T, Okura Y, Hamabe Y. Epidemiological state, predictive model for mortality, and optimal management strategy for pancreatic injury: A multicentre nationwide cohort study. Injury 2020;51:59-65. https://doi.org/10.1016/j.injury.2019.08.009
Rodriguez F, García A, Ordoñez C, Vernaza C, Herrera JP, Puyana JC. Trauma Pancreático Penetrante Severo-Revisión Retrospectiva de Una Serie de Casos Manejados Con Una Estrategia Simplificada en un Centro de Trauma Nivel 1. Panam J Trauma, Crit Care Emerg Surg 2015;4:147-54. https://doi.org/10.5005/jp-journals-10030-1129
Panda A, Kumar A, Gamanagatti S, Bhalla AS, Sharma R, Kumar S, et al. Evaluation of diagnostic utility of multidetector computed tomography and magnetic resonance imaging in blunt pancreatic trauma: A prospective study. Acta Radiol 2015;56:387-96. https://doi.org/10.1177/0284185114529949
Potoka DA, Gaines BA, Leppäniemi A, Peitzman AB. Management of blunt pancreatic trauma: what's new? Eur J Trauma Emerg Surg 2015;41:239-50. https://doi.org/10.1007/s00068-015-0510-3
Schellenberg M, Inaba K, Bardes JM, Cheng V, Matsushima K, Lam L, et al. Detection of traumatic pancreatic duct disruption in the modern era. Am J Surg 2018;216:299-303. https://doi.org/10.1016/j.amjsurg.2018.06.002
Osborn LA, Brenner ML, Prater SJ, Moore LJ. Resuscitative endovascular balloon occlusion of the aorta: Current evidence. Open Access Emerg Med 2019;11:29-38. https://doi.org/10.2147/OAEM.S166087.
Ordoñez CA, Parra M, Caicedo Y, Padilla N, Rodriguez F, Serna JJ, et al. REBOA as a New Damage Control Component in Hemodynamically Unstable NTCH patients. Colomb Med (Cali). 2020; 51(4): e-4014353. https://doi.org/10.25100/cm.v51i4.4353
Girard E, Abba J, Arvieux C, Trilling B, Sage PY, Mougin N, et al. Management of pancreatic trauma. J Visc Surg 2016;153:259-68. https://doi.org/10.1016/j.jviscsurg.2016.02.006
de Carvalho MEAJ, Cunha AG. Pancreaticodudonectomy in trauma: One or two stages? Injury. 2020; 51: 592-6. https://doi.org/10.1016/j.injury.2020.01.018
Krige J, Nicol A, Navsaria P. Treating complex pancreatic injuries. Trauma and pancreatic surgeons working together is the modern management paradigm. J Visc Surg 2017;154:143. https://doi.org/10.1016/j.jviscsurg.2017.02.002
Byrge N, Heilbrun M, Winkler N, Sommers D, Evans H, Cattin LM, et al. An AAST-MITC analysis of pancreatic trauma: Staple or sew? Resect or drain? J Trauma Acute Care Surg. 2018; 85(3): 435-443. https://doi.org/10.1097/TA.0000000000001987
Asensio JA, Petrone P, Roldán G, Kuncir E, Demetriades D. Pancreaticoduodenectomy: A rare procedure for the management of complex pancreaticoduodenal injuries. J Am Coll Surg 2003. https://doi.org/10.1016/j.jamcollsurg.2003.07.019
Vasquez JC, Coimbra R, Hoyt DB, Fortlage D. Management of penetrating pancreatic trauma: An 11-year experience of a level-1 trauma center. Injury 2001. https://doi.org/10.1016/S0020-1383(01)00099-7
Ball CG, Correa-Gallego C, Howard TJ, Zyromski NJ, Lillemoe KD. Damage Control Principles for Pancreatic Surgery. J Gastrointest Surg 2010;14:1632-3. https://doi.org/10.1007/s11605-010-1286-8
Ordoñez CA, Badiel M, Pino LF, Salamea JC, Loaiza JH, Parra MW, et al. Damage control resuscitation: Early decision strategies in abdominal gunshot wounds using an easy "aBCD" mnemonic. J Trauma Acute Care Surg. 2012; 73:1074-8. https://doi.org/10.1097/TA.0b013e31826fc780
Moore E, Cogbill T, Malangoni M, Jurkovich G, Champion H, Gennarelli T, et al. Organ injury scaling, II: pancreas, duodenum, small bowel, colon and rectum. J Trauma 1990;30:1427-9. https://doi.org/10.1097/00005373-199011000-00035
Copyright (c) 2020 carlos ordoñez, Michael Parra, Mauricio Millan, Yaset Caicedo, Natalia Padilla, Alberto Garcia, Adolfo Gonzalez, Luis Fernando Pino, Fernando Rodriguez, Jose Julian Serna, Alexander Salcedo, Ricardo Ferrada, Rao Ivatury, Fernando Miñan (Author)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-4495-7405
https://orcid.org/0000-0003-4495-7405


















