Damage control in penetrating cardiac trauma
Abstract
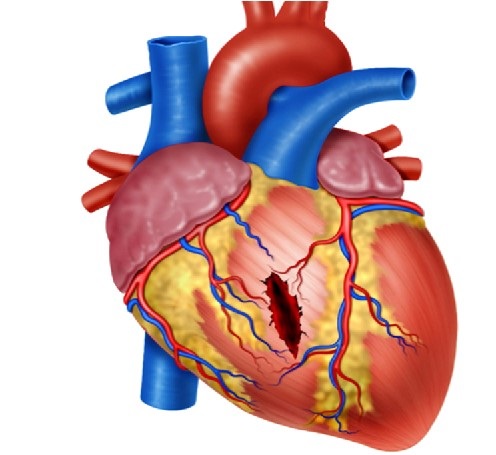
Definitive management of hemodynamically stable patients with penetrating cardiac injuries remains controversial between those who propose aggressive invasive care versus those who opt for a less invasive or non-operative approach. This controversy even extends to cases of hemodynamically unstable patients in which damage control surgery is thought to be useful and effective. The aim of this article is to delineate our experience in the surgical management of penetrating cardiac injuries via the creation of a clear and practical algorithm that includes basic principles of damage control surgery. We recommend that all patients with precordial penetrating injuries undergo trans-thoracic ultrasound screening as an integral component of their initial evaluation. In those patients who arrive hemodynamically stable but have a positive ultrasound, a pericardial window with lavage and drainage should follow. We want to emphasize the importance of the pericardial lavage and drainage in the surgical management algorithm of these patients. Before this concept, all positive pericardial windows ended up in an open chest exploration. With the coming of the pericardial lavage and drainage procedure, the reported literature and our experience have shown that 25% of positive pericardial windows do not benefit and/or require further invasive procedures. However, in hemodynamically unstable patients, damage control surgery may still be required to control ongoing bleeding. For this purpose, we propose a surgical management algorithm that includes all of these essential clinical aspects in the care of these patients.
Authors
Downloads
Keywords
- Thoracic Ultrasound
- Damage Control Surgery
- Penetrating cardiac trauma
- cardiac tamponade
- thoracotomy
- advanced trauma life support care
- negative-pressure wound therapy
- pericardiectomy
- hemothorax
- chest tubes
- pneumothorax
- pericardial window techniques
References
Morse BC, Mina MJ, Carr JS, Jhunjhunwala R, Dente CJ, Zink JU, et al. Penetrating cardiac injuries: A 36-year perspective at an urban, Level i trauma center. J Trauma Acute Care Surg 2016;81:623–31. https://doi.org/10.1097/TA.0000000000001165.
Degiannis E, Bowley DM, Westaby S. Penetrating cardiac injury. Ann R Coll Surg Engl 2005;87:61–3. https://doi.org/10.1308/1478708051207.
Mugala DD, Makupe A, Ziddulla, Sakala D, Simon M, Chibale B, et al. Occurrence of penetrating chest and hearts injury following assaults: a presentation of two cases. MOJ Clin Med Case Reports 2018;8:88–94. https://doi.org/10.15406/mojcr.2018.08.00247.
Andrade-Alegre R. Trauma Cardíaco Penetrante. Panam J Trauma 2004;11:50–8. https://doi.org/10.1017/CBO9781107415324.004.
Nicol AJ. Cardiac Hemorrhage: Treatment of the Bleeding Heart. In: Ball CG, Dixon E, editors. Treat. Ongoing Hemorrhage Art Cr. Stopping Sev. Bleeding, 2018, p. 67–80.
Sanchez AI, Garcia A, Velazquez M, Puyana JC. Predictors of positive subxiphoid pericardial window in stable patients with penetrating injuries to the precordial region. Panam J Trauma 2016;5:43–51. https://doi.org/10.5005/jp-journals-10030-1142.
Wall MJ, Mattox KL, Chen CD, Baldwin JC. Acute management of complex cardiac injuries. J. Trauma - Inj. Infect. Crit. Care, vol. 42, J Trauma; 1997, p. 905–12. https://doi.org/10.1097/00005373-199705000-00022.
Isaza-Restrepo A, Bolívar-Sáenz DJ, Tarazona-Lara M, Tovar JR. Penetrating cardiac trauma: Analysis of 240 cases from a hospital in Bogota, Colombia. World J Emerg Surg 2017;12. https://doi.org/10.1186/s13017-017-0138-1.
García A. Enfoque inicial del paciente estable con trauma precordial penetrante: ¿es tiempo de un cambio? Rev Colomb Cirugía 2019;34:16–24. https://doi.org/10.30944/20117582.93.
Ingraham A, Sperry J. Operative Management of Cardiac Injuries: Diagnosis, Technique, and Postoperative Complications. Curr Trauma Reports 2015;1:225–31. https://doi.org/10.1007/s40719-015-0032-9.
Gonzalez-Hadad A, García AF, Serna JJ, Herrera MA, Morales M, Manzano-Nunez R. The Role of Ultrasound for Detecting Occult Penetrating Cardiac Wounds in Hemodynamically Stable Patients. World J Surg 2020;44:1673–80. https://doi.org/10.1007/s00268-020-05376-7.
Moore EE, Malangoni MA, Cogbill TH, Shackford SR, Champion HR, Jurkovich GJ, et al. Organ injury scaling. IV: Thoracic vascular, lung, cardiac, and diaphragm. J Trauma 1994;36:299–300.
Ditzel RM, Anderson JL, Eisenhart WJ, Rankin CJ, DeFeo DR, Oak S, et al. A review of transfusion- And trauma-induced hypocalcemia: Is it time to change the lethal triad to the lethal diamond? J Trauma Acute Care Surg 2020;88:434–9. https://doi.org/10.1097/TA.0000000000002570.
Ordoñez CA, Parra MW, Serna JJ, Rodríguez H F, García AF, Salcedo A, et al. Damage Control Resuscitation : REBOA as the New Fourth pillar. Colomb Med 2020. https://doi.org/10.25100/cm.v51i4.4353.
Wandling MW, An GC. A case report of thoracic compartment syndrome in the setting of penetrating chest trauma and review of the literature. World J Emerg Surg 2010;5:1–5. https://doi.org/10.1186/1749-7922-5-22.
Onem G, Baltalarli A, Sungurtekin H, Evrengul H, Ozcan AV, Kaya S, et al. Iatrogenic cardiac herniation and torsion after surgery for a penetrating cardiac injury. Texas Hear Inst J 2006;33:526–8.
Rendón F, Gómez Danés LH, Castro M. Delayed cardiac tamponade after penetrating thoracic trauma. Asian Cardiovasc Thorac Ann 2004;12:139–42. https://doi.org/10.1177/021849230401200212.
Van Waes OJF, Halm JA, Van Imhoff DI, Navsaria PH, Nicol AJ, Verhofstad MHJ, et al. Selective non-operative management of penetrating thoracic injury. Eur J Emerg Med 2018;25:32–8. https://doi.org/10.1097/MEJ.0000000000000401.
Brewster SA, Thirlby RC, Snyder WH. Subxiphoid Pericardial Window and Penetrating Cardiac Trauma. Arch Surg 1988;123:937–41. https://doi.org/10.1001/archsurg.1988.01400320023003.
Saranteas T, Mavrogenis AF, Mandila C, Poularas J, Panou F. Ultrasound in cardiac trauma. J Crit Care 2017;38:144–51. https://doi.org/10.1016/j.jcrc.2016.10.032.
Nicol AJ, Navsaria PH, Beningfield S, Hommes M, Kahn D. Screening for occult penetrating cardiac injuries. Ann Surg 2015;261:573–8. https://doi.org/10.1097/SLA.0000000000000713.
Ball CG, Williams BH, Wyrzykowski AD, Nicholas JM, Rozycki GS, Feliciano D V. A caveat to the performance of pericardial ultrasound in patients with penetrating cardiac wounds. J Trauma - Inj Infect Crit Care 2009;67:1123–4. https://doi.org/10.1097/TA.0b013e3181b16f30.
Chestovich PJ, McNicoll CF, Fraser DR, Patel PP, Kuhls DA, Clark E, et al. Selective use of pericardial window and drainage as sole treatment for hemopericardium from penetrating chest trauma. Trauma Surg Acute Care Open 2018;3:e000187. https://doi.org/10.1136/tsaco-2018-000187.
Nicol AJ, Navsaria P, Hommes M, Ball C, Edu S, Kahn D. Sternotomy or Drainage for a Hemopericardium After Penetrating Trauma: A Safe Procedure? Ann Surg 2016;263:e32. https://doi.org/10.1097/SLA.0000000000001146.
Nicol AJ, Navsaria PH, Hommes M, Ball CG, Edu S, Kahn D. Sternotomy or drainage for a hemopericardium after penetrating trauma: A randomized controlled trial. Ann Surg 2014;259:438–42. https://doi.org/10.1097/SLA.0b013e31829069a1.
Copyright (c) 2021 Universidad del Valle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0001-5862-4906
https://orcid.org/0000-0001-5862-4906


















