Whole Blood for Blood Loss: Hemostatic Resuscitation in Damage Control
Abstract
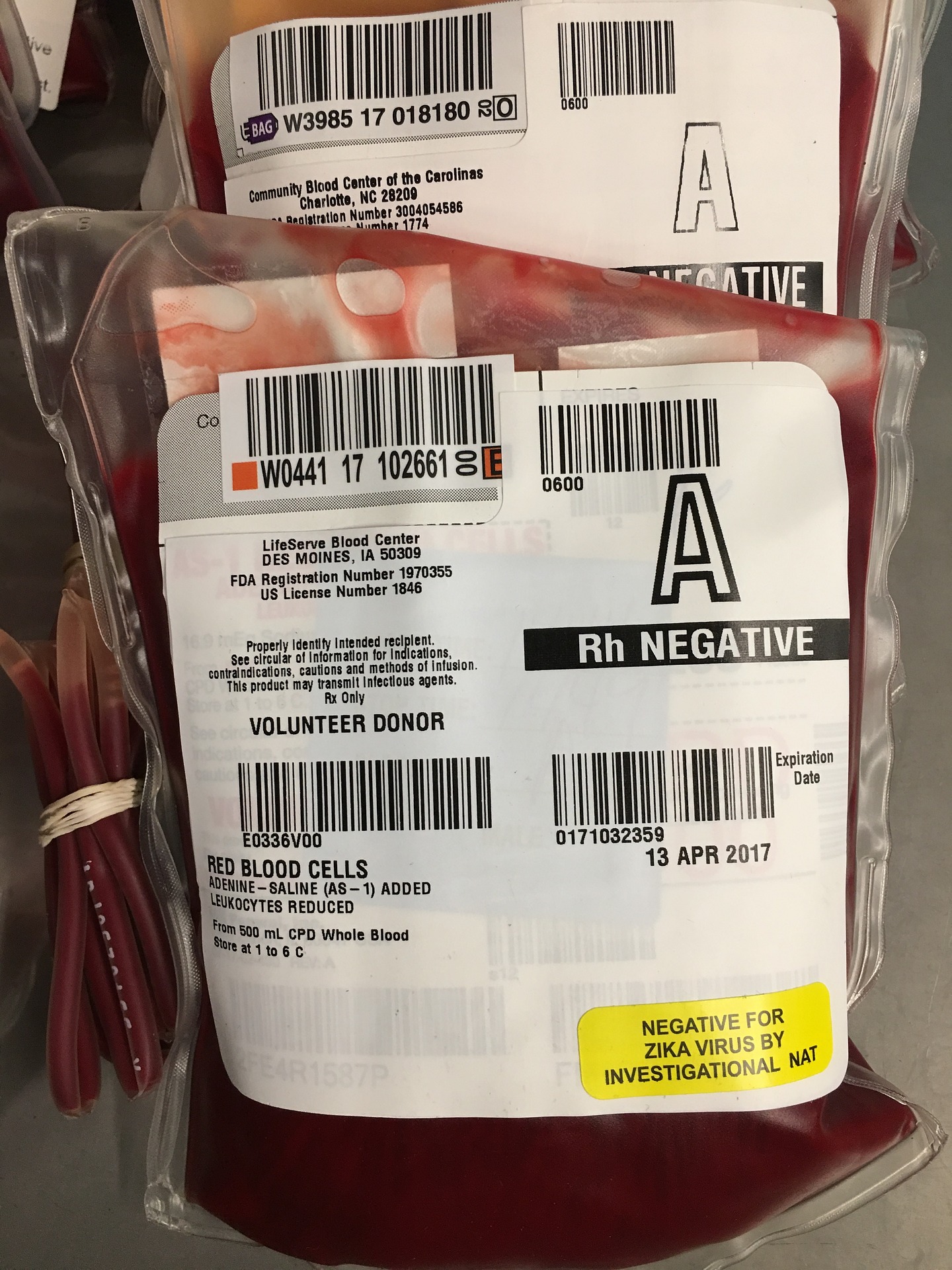
Hemorrhagic shock and its complications are a major cause of death among trauma patients. The management of hemorrhagic shock using a damage control resuscitation strategy has been shown to decrease mortality and improve patient outcomes. One of the components of damage control resuscitation is hemostatic resuscitation, which involves the replacement of lost blood volume with components such as packed red blood cells, fresh frozen plasma, cryoprecipitate, and platelets in a 1:1:1:1 ratio. However, this is a strategy that is not applicable in many parts of Latin America and other low-and-middle-income countries throughout the world, where there is a lack of well-equipped blood banks and an insufficient availability of blood products. To overcome these barriers, we propose the use of cold fresh whole blood for hemostatic resuscitation in exsanguinating patients. Over 6 years of experience in Ecuador has shown that resuscitation with cold fresh whole blood has similar outcomes and a similar safety profile compared to resuscitation with hemocomponents. Whole blood confers many advantages over component therapy including, but not limited to the transfusion of blood with a physiologic ratio of components, ease of transport and transfusion, less volume of anticoagulants and additives transfused to the patient, and exposure to fewer donors. Whole blood is a tool with reemerging potential that can be implemented in civilian trauma centers with optimal results and less technical demand.
Authors
Downloads
Keywords
- Whole Blood
- Transfusion
- Whole Blood for Blood Loss
- Crystalloid Solutions
- Shock, Hemorrhagic
- Disseminated Intravascular Coagulation
- Trauma Centers
- Blood Safety
- Hemostatics
- Hypothermia
- Hypocalcemia
- Blood Coagulation Factors
- Respiratory Distress Syndrome
- Compartment Syndromes
References
Eastridge BJ, Holcomb JB, Shackelford S. Outcomes of traumatic hemorrhagic shock and the epidemiology of preventable death from injury. Transfusion. 2019;59(S2):1423-8. https://doi.org/10.1111/trf.15161
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471-82. https://doi.org/10.1001/jama.2015.12
Moore SE, Decker A, Hubbard A, Callcut RA, Fox EE, Del Junco DJ, et al. Statistical Machines for Trauma Hospital Outcomes Research: Application to the PRospective, Observational, Multi-Center Major Trauma Transfusion (PROMMTT) Study. PLoS One. 2015;10(8):e0136438. https://doi.org/10.1371/journal.pone.0136438
Spinella PC, Pidcoke HF, Strandenes G, Hervig T, Fisher A, Jenkins D, et al. Whole blood for hemostatic resuscitation of major bleeding. Transfusion. 2016;56 Suppl 2:S190-202. https://doi.org/10.1111/trf.13491
Cap AP, Pidcoke HF, Spinella P, Strandenes G, Borgman MA, Schreiber M, et al. Damage Control Resuscitation. Mil Med. 2018;183(suppl_2):36-43. https://doi.org/10.1093/milmed/usy112
Chang R, Holcomb JB. Optimal Fluid Therapy for Traumatic Hemorrhagic Shock. Crit Care Clin. 2017;33(1):15-36. https://doi.org/10.1016/j.ccc.2016.08.007
Woolley T, Thompson P, Kirkman E, Reed R, Ausset S, Beckett A, et al. Trauma Hemostasis and Oxygenation Research Network position paper on the role of hypotensive resuscitation as part of remote damage control resuscitation. J Trauma Acute Care Surg. 2018;84(6S Suppl 1):S3-S13. https://doi.org/10.1097/TA.0000000000001856
Ordoñez CA, Badiel M, Pino LF, Salamea JC, Loaiza JH, Parra MW, et al. Damage control resuscitation: early decision strategies in abdominal gunshot wounds using an easy "ABCD" mnemonic. J Trauma Acute Care Surg. 2012;73(5):1074-8. https://doi.org/10.1097/TA.0b013e31826fc780
Holcomb JB, Fox EE, Wade CE, Group PS. The PRospective Observational Multicenter Major Trauma Transfusion (PROMMTT) study. J Trauma Acute Care Surg. 2013;75(1 Suppl 1):S1-2. https://doi.org/10.1097/TA.0b013e3182983876
Brown JB, Guyette FX, Neal MD, Claridge JA, Daley BJ, Harbrecht BG, et al. Taking the Blood Bank to the Field: The Design and Rationale of the Prehospital Air Medical Plasma (PAMPer) Trial. Prehosp Emerg Care. 2015;19(3):343-50. https://doi.org/10.3109/10903127.2014.995851
Spinella PC, Cap AP. Whole blood: back to the future. Curr Opin Hematol. 2016;23(6):536-42. https://doi.org/10.1097/MOH.0000000000000284
Cap AP, Beckett A, Benov A, Borgman M, Chen J, Corley JB, et al. Whole Blood Transfusion. Mil Med. 2018;183(suppl_2):44-51. https://doi.org/10.1093/milmed/usy120
Muñoz-Valencia A, Bonilla-Escobar F, Puyana JC, editors. Effect of Blood Bank Availability on Mortality Due to Shock after Trauma in a Middle-Income Country. American College of Surgeons; 2019; San Francisco, CA. https://doi.org/10.1016/j.jamcollsurg.2019.08.288
Roberts N, James S, Delaney M, Fitzmaurice C. The global need and availability of blood products: a modelling study. Lancet Haematol. 2019;6(12):e606-e15. https://doi.org/10.1016/S2352-3026(19)30200-5
Blood safety and availability: The World Health Organization; 2019 [Available from: https://www.who.int/news-room/fact-sheets/detail/blood-safety-and-availability.
Latin America and the Caribbean approaching half-way mark toward goal of 100% voluntary blood donation: Pan American Health Association; 2016 [Available from: https://www.paho.org/salud-en-las-americas-2017/?tag=en.
Supply of Blood for Transfusion in Latin American and Caribbean Countries 2014 and 2015 Washington D.C.: Pan American Health Organization; 2017.
MacLeod JB, Lynn M, McKenney MG, Cohn SM, Murtha M. Early coagulopathy predicts mortality in trauma. J Trauma. 2003;55(1):39-44. https://doi.org/10.1097/01.TA.0000075338.21177.EF
Kushimoto S, Kudo D, Kawazoe Y. Acute traumatic coagulopathy and trauma-induced coagulopathy: an overview. Journal of Intensive Care. 2017;5(6). https://doi.org/10.1186/s40560-016-0196-6
Mizobata Y. Damage control resuscitation: a practical approach for severely hemorrhagic patients and its effects on trauma surgery. Journal of Intensive Care. 2017;5(4). https://doi.org/10.1186/s40560-016-0197-5
Ditzel RM, Anderson JL, Eisenhart WJ, Rankin CJ, DeFeo DR, Oak S, et al. A review of transfusion- and trauma-induced hypocalcemia: Is it time to change the lethal triad to the lethal diamond? J Trauma Acute Care Surg. 2020;88(3):434-9. https://doi.org/10.1097/TA.0000000000002570
Ordoñez CA, Parra MW, Serna JJ, Rodríguez H F, García AF, Salcedo A, et al. Damage Control Resuscitation : REBOA as the New Fourth pillar. Colomb Med 2020. https://doi.org/10.25100/cm.v51i4.4353.
Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94(6):1176-86. https://doi.org/10.1378/chest.94.6.1176
Kasotakis G, Sideris A, Yang Y, de Moya M, Alam H, King DR, et al. Aggressive early crystalloid resuscitation adversely affects outcomes in adult blunt trauma patients: an analysis of the Glue Grant database. J Trauma Acute Care Surg. 2013;74(5):1215-21; discussion 21-2.
Bickell WH, Wall MJ, Pepe PE, Martin RR, Ginger VF, Allen MK, et al. Immediate versus delayed fluid resuscitation for hypotensive patients with penetrating torso injuries. N Engl J Med. 1994;331(17):1105-9. https://doi.org/10.1056/NEJM199410273311701
Ley EJ, Clond MA, Srour MK, Barnajian M, Mirocha J, Margulies DR, et al. Emergency department crystalloid resuscitation of 1.5 L or more is associated with increased mortality in elderly and nonelderly trauma patients. J Trauma. 2011;70(2):398-400. https://doi.org/10.1097/TA.0b013e318208f99b
Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007;63(4):805-13. https://doi.org/10.1097/TA.0b013e3181271ba3
Savage SA, Zarzaur BL, Croce MA, Fabian TC. Redefining massive transfusion when every second counts. J Trauma Acute Care Surg. 2013;74(2):396-400; discussion -2. https://doi.org/10.1097/TA.0b013e31827a3639
Pommerening MJ, Goodman MD, Holcomb JB, Wade CE, Fox EE, Del Junco DJ, et al. Clinical gestalt and the prediction of massive transfusion after trauma. Injury. 2015;46(5):807-13. https://doi.org/10.1016/j.injury.2014.12.026
Johansson PI, Stissing T, Bochsen L, Ostrowski SR. Thrombelastography and tromboelastometry in assessing coagulopathy in trauma. Scand J Trauma Resusc Emerg Med. 2009;17:45. https://doi.org/10.1186/1757-7241-17-45
Hunt H, Stanworth S, Curry N, Woolley T, Cooper C, Ukoumunne O, et al. Thromboelastography (TEG) and rotational thromboelastometry (ROTEM) for trauma induced coagulopathy in adult trauma patients with bleeding. Cochrane Database Syst Rev. 2015(2):CD010438. https://doi.org/10.1002/14651858.CD010438.pub2
Gonzalez E, Moore EE, Moore HB. Management of Trauma-Induced Coagulopathy with Thrombelastography. Crit Care Clin. 2017;33(1):119-34. https://doi.org/10.1016/j.ccc.2016.09.002
Spinella PC, Perkins JG, Grathwohl KW, Beekley AC, Holcomb JB. Warm fresh whole blood is independently associated with improved survival for patients with combat-related traumatic injuries. J Trauma. 2009;66(4 Suppl):S69-76. https://doi.org/10.1097/TA.0b013e31819d85fb
Yazer MH, Cap AP, Spinella PC. Raising the standards on whole blood. J Trauma Acute Care Surg. 2018;84(6S Suppl 1):S14-S7. https://doi.org/10.1097/TA.0000000000001778
Hess JR. Resuscitation of trauma-induced coagulopathy. Hematology Am Soc Hematol Educ Program. 2013;2013:664-7. https://doi.org/10.1182/asheducation-2013.1.664
Sarmiento Altamirano D, Himmler A, Chango Sigüenza O, Pino Andrade R, Flores Lazo N, Reinoso Naranjo J, et al. The Successful Implementation of a Trauma and Acute Care Surgery Model in Ecuador. World J Surg. 2020. https://doi.org/10.1007/s00268-020-05435-z
Himmler A, Galarza M, Reinoso J, Peña S, Sarmiento D, Flores N, et al. Is the whole greater than the sum of its parts? The implementation and outcomes of a whole blood program in Ecuador. Res. Sq., 2020, p. 14. https://doi.org/10.21203/rs.3.rs-66244/v1.
Perkins JG, Cap AP, Spinella PC, Shorr AF, Beekley AC, Grathwohl KW, et al. Comparison of platelet transfusion as fresh whole blood versus apheresis platelets for massively transfused combat trauma patients (CME). Transfusion. 2011;51(2):242-52. https://doi.org/10.1111/j.1537-2995.2010.02818.x
Nessen SC, Eastridge BJ, Cronk D, Craig RM, Berséus O, Ellison R, et al. Fresh whole blood use by forward surgical teams in Afghanistan is associated with improved survival compared to component therapy without platelets. Transfusion. 2013;53 Suppl 1:107S-13S. https://doi.org/10.1111/trf.12044
Ho KM, Leonard AD. Lack of effect of unrefrigerated young whole blood transfusion on patient outcomes after massive transfusion in a civilian setting. Transfusion. 2011;51(8):1669-75. https://doi.org/10.1111/j.1537-2995.2010.02975.x
Cotton BA, Podbielski J, Camp E, Welch T, del Junco D, Bai Y, et al. A randomized controlled pilot trial of modified whole blood versus component therapy in severely injured patients requiring large volume transfusions. Ann Surg. 2013;258(4):527-32; discussion 32-3. https://doi.org/10.1097/SLA.0b013e3182a4ffa0
Hazelton JP, Cannon JW, Zatorski C, Roman JS, Moore SA, Young AJ, et al. Cold-stored whole blood: A better method of trauma resuscitation? J Trauma Acute Care Surg. 2019;87(5):1035-41. https://doi.org/10.1097/TA.0000000000002471
Williams J, Merutka N, Meyer D, Bai Y, Prater S, Cabrera R, et al. Safety profile and impact of low-titer group O whole blood for emergency use in trauma. J Trauma Acute Care Surg. 2020;88(1):87-93. https://doi.org/10.1097/TA.0000000000002498
Yazer MH, Jackson B, Sperry JL, Alarcon L, Triulzi DJ, Murdock AD. Initial safety and feasibility of cold-stored uncrossmatched whole blood transfusion in civilian trauma patients. J Trauma Acute Care Surg. 2016;81(1):21-6. https://doi.org/10.1097/TA.0000000000001100
Seheult JN, Anto V, Alarcon LH, Sperry JL, Triulzi DJ, Yazer MH. Clinical outcomes among low-titer group O whole blood recipients compared to recipients of conventional components in civilian trauma resuscitation. Transfusion. 2018;58(8):1838-45. https://doi.org/10.1111/trf.14779
Rhee P, Inaba K, Pandit V, Khalil M, Siboni S, Vercruysse G, et al. Early autologous fresh whole blood transfusion leads to less allogeneic transfusions and is safe. J Trauma Acute Care Surg. 2015;78(4):729-34. https://doi.org/10.1097/TA.0000000000000599
Folkersen L, Tang M, Grunnet N, Jakobsen CJ. Transfusion of shed mediastinal blood reduces the use of allogenic blood transfusion without increasing complications. Perfusion. 2011;26(2):145-50. https://doi.org/10.1177/0267659110393299
Bahr MP, Yazer MH, Triulzi DJ, Collins RA. Whole blood for the acutely haemorrhaging civilian trauma patient: a novel idea or rediscovery? Transfus Med. 2016;26(6):406-14. https://doi.org/10.1111/tme.12329
Macia C, Guzmán M, Hernández E, Alcala M, García A, Caicedo Y, et al. Whole Blood Prepared via a Platelet-Sparing Leukoreduction Filtration System Preserves the Hemostatic Function for 21 Days: Early Results of a Pilot Study to Expand the Use of Whole Blood for Trauma in South America. J Am Coll Surg 2020;231:e64. https://doi.org/10.1016/j.jamcollsurg.2020.08.156.
Seheult JN, Triulzi DJ, Alarcon LH, Sperry JL, Murdock A, Yazer MH. Measurement of haemolysis markers following transfusion of uncrossmatched, low-titre, group O+ whole blood in civilian trauma patients: initial experience at a level 1 trauma centre. Transfus Med. 2017;27(1):30-5. https://doi.org/10.1111/tme.12372
Copyright (c) 2020 Universidad del Valle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0002-9084-3030
https://orcid.org/0000-0002-9084-3030


















