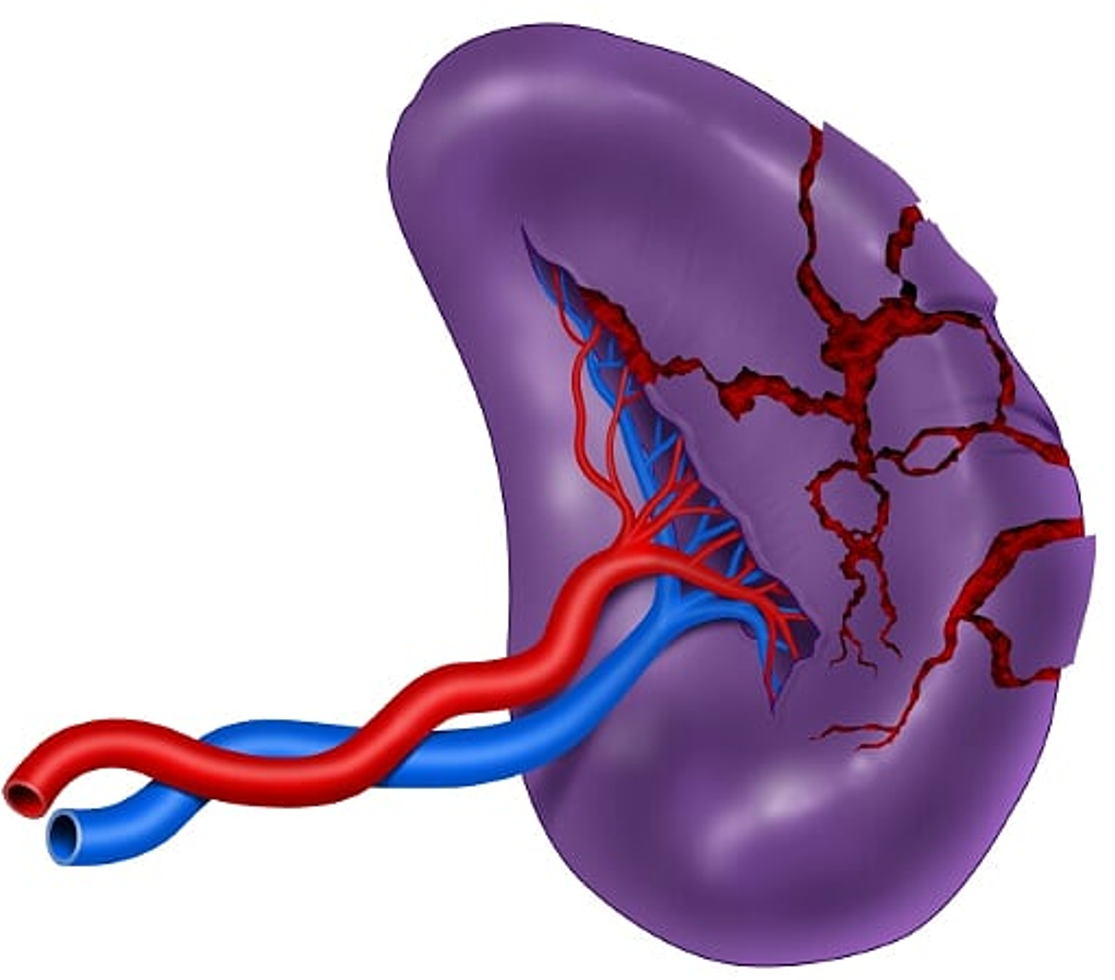
Damage control surgery for splenic trauma: "preserve an organ - preserve a life"
Abstract
The spleen is one of the most commonly injured solid organs of the abdominal cavity and an early diagnosis can reduce the associated mortality. Over the past couple of decades, management of splenic injuries has evolved to a prefered non-operative approach even in severely injured cases. However, the optimal surgical management of splenic trauma in severely injured patients remains controversial. This article aims to present an algorithm for the management of splenic trauma in severely injured patients, that includes basic principles of damage control surgery and is based on the experience obtained by the Trauma and Emergency Surgery Group (CTE) of Cali, Colombia. The choice between a conservative or a surgical approach depends on the hemodynamic status of the patient. In hemodynamically stable patients, a computed tomography angiogram should be performed to determine if non-operative management is feasible and if angioembolization is required. While hemodynamically unstable patients should be transferred immediately to the operating room for damage control surgery, which includes splenic packing and placement of a negative pressure dressing, followed by angiography with embolization of any ongoing arterial bleeding. It is our recommendation that both damage control principles and emerging endovascular technologies should be applied to achieve splenic salvage when possible. However, if surgical bleeding persists a splenectomy may be required as a definitive lifesaving maneuver.
Authors
Downloads
Keywords
- Injury Severity Score
- Spleen
- Splenectomy
- Focused Assessment with Sonography for Trauma
- Laparotomy
- Negative-Pressure Wound Therapy
- Angiography
- Balloon Occlusion
- Vascular Access Devices
- REBOA
- Damage Control Surgery
References
Forsythe RM, Harbrecht BG, Peitzman AB. Blunt splenic trauma. Scand J Surg 2006;95:146-51. https://doi.org/10.1177/145749690609500303.
Cales RH. Preventable trauma deaths. A review of trauma care systems development. JAMA J Am Med Assoc 1985;254:1059-63. https://doi.org/10.1001/jama.254.8.1059.
Olthof DC, Van Der Vlies CH, Joosse P, Van Delden OM, Jurkovich GJ, Goslings JC. Consensus strategies for the nonoperative management of patients with blunt splenic injury: A Delphi study. J Trauma Acute Care Surg 2013;74:1567-74. https://doi.org/10.1097/TA.0b013e3182921627.
Petrone P, Peña MFA, Staffolani MJS, Brathwaite C, Axelrad A, Esparragón JC. Evolución en el tratamiento conservador del traumatismo esplénico contuso. Cirugía Española 2017;95:420-7. https://doi.org/10.1016/j.ciresp.2017.07.007
Coccolini F, Montori G, Catena F, Kluger Y, Biffl W, Moore EE, et al. Splenic trauma: WSES classification and guidelines for adult and pediatric patients. World J Emerg Surg 2017;12. https://doi.org/10.1186/s13017-017-0151-4.
Coccolini F, Fugazzola P, Morganti L, Ceresoli M, Magnone S, Montori G, et al. The World Society of Emergency Surgery (WSES) spleen trauma classification: A useful tool in the management of splenic trauma. World J Emerg Surg 2019;14:30. https://doi.org/10.1186/s13017-019-0246-1.
Teuben M, Spijkerman R, Pfeifer R, Blokhuis T, Huige J, Pape HC, et al. Selective non-operative management for penetrating splenic trauma: a systematic review. Eur J Trauma Emerg Surg 2019;45:979-85. https://doi.org/10.1007/s00068-019-01117-1.
Ordoñez CA, Badiel M, Pino LF, Salamea JC, Loaiza JH, Parra MW, et al. Damage control resuscitation: Early decision strategies in abdominal gunshot wounds using an easy "aBCD" mnemonic. J Trauma Acute Care Surg 2012;73:1074-8. https://doi.org/10.1097/TA.0b013e31826fc780.
Ordoñez CA, Herrera-Escobar JP, Parra MW, Rodriguez-Ossa PA, Mejia DA, Sanchez AI, et al. Computed tomography in hemodynamically unstable severely injured blunt and penetrating trauma patients. J Trauma Acute Care Surg 2016;80:597-603. https://doi.org/10.1097/TA.0000000000000975.
Ordoñez C, Garcia AF, Parra M, Valle AM del, Herrera-Escobar JP, Guzman-Rodriguez M, et al. Single-pass Whole-body vs Organ-selective Computed Tomography for Trauma: Timely Diagnosis vs Radiation Exposure: An Observational Study. Panam J Trauma, Crit Care Emerg Surg 2020;9:26-31. https://doi.org/10.5005/jp-journals-10030-1262.
Ordoñez CA, García C, Parra MW, Angamarca E, Guzmán-Rodríguez M, Orlas CP, et al. Implementation of a new single-pass whole-body computed tomography protocol: Is it safe, effective and efficient in patients with severe trauma? Colomb Med 2020;51:1-10. https://doi.org/10.25100/cm.v51i1.4224.
Shapiro MJ, Krausz C, Durham RM, Mazuski JE. Overuse of splenic scoring and computed tomographic scans. J Trauma - Inj Infect Crit Care 1999;47:651-8. https://doi.org/10.1097/00005373-199910000-00008.
Rosati C, Ata A, Siskin GP, Megna D, Bonville DJ, Stain SC. Management of splenic trauma: A single institution's 8-year experience. Am J Surg 2015;209:308-14. https://doi.org/10.1016/j.amjsurg.2014.06.034.
Banerjee A, Duane TM, Wilson SP, Haney S, O'Neill PJ, Evans HL, et al. Trauma center variation in splenic artery embolization and spleen salvage: A multicenter analysis. J Trauma Acute Care Surg 2013;75:69-75. https://doi.org/10.1097/TA.0b013e3182988b3b.
Requarth JA, D'Agostino RB, Miller PR. Nonoperative management of adult blunt splenic injury with and without splenic artery embolotherapy: A meta-analysis. J Trauma - Inj Infect Crit Care 2011;71:898-903. https://doi.org/10.1097/TA.0b013e318227ea50.
Ordoñez C, Pino L, Badiel M, Sanchez A, Loaiza J, Ramirez O, et al. The 1-2-3 approach to abdominal packing. World J Surg 2012;36:2761-6. https://doi.org/10.1007/s00268-012-1745-3.
https://doi.org/10.1007/s00268-012-1745-3
Ordoñez CA, Rodríguez F, Parra M, Herrera JP, Guzmán-Rodríguez M, Orlas C, et al. Resuscitative endovascular balloon of the aorta is feasible in penetrating chest trauma with major hemorrhage: Proposal of a new institutional deployment algorithm. J Trauma Acute Care Surg 2020;89:311-9. https://doi.org/10.1097/ta.0000000000002773.
McIntyre LK, Schiff M, Jurkovich GJ, Weigelt J, Asensio JA, Cogbill TH, et al. Failure of nonoperative management of splenic injuries: Causes and consequences. Arch Surg 2005;140:563-9. https://doi.org/10.1001/archsurg.140.6.563.
Peitzman AB, Harbrecht BG, Rivera L, Heil B. Failure of observation of blunt splenic injury in adults: Variability in practice and adverse consequences. J Am Coll Surg 2005;201:179-87. https://doi.org/10.1016/j.jamcollsurg.2005.03.037.
Smith J, Armen S, Cook CH, Martin LC. Blunt splenic injuries: Have we watched long enough? J Trauma - Inj Infect Crit Care 2008;64:656-63. https://doi.org/10.1097/TA.0b013e3181650fb4.
Bee TK, Croce MA, Miller PR, Pritchard FE, Davis KA, Fabian TC. Failures of splenic nonoperative management: Is the glass half empty or half full? J Trauma - Inj Infect Crit Care 2001;50:230-6. https://doi.org/10.1097/00005373-200102000-00007.
Jeremitsky E, Smith RS, Ong AW. Starting the clock: Defining nonoperative management of blunt splenic injury by time. Am J Surg 2013;205:298-301. https://doi.org/10.1016/j.amjsurg.2012.10.022.
Plurad DS, Green DJ, Inaba K, Benfield R, Lam L, Putty B, et al. Blunt assault is associated with failure of nonoperative management of the spleen independent of organ injury grade and despite lower overall injury severity. J Trauma - Inj Infect Crit Care 2009;66:630-5. https://doi.org/10.1097/TA.0b013e3181991aed.
Peitzman AB, Heil B, Rivera L, Federle MB, Harbrecht BG, Clancy KD, et al. Blunt splenic injury in adults: Multi-institutional study of the Eastern Association for the Surgery of Trauma. J Trauma - Inj Infect Crit Care 2000;49:177-89. https://doi.org/10.1097/00005373-200008000-00002.
Smith HE, Biffl WL, Majercik SD, Jednacz J, Lambiase R, Cioffi WG. Splenic artery embolization: Have we gone too far? J Trauma - Inj Infect Crit Care 2006;61:541-4. https://doi.org/10.1097/01.ta.0000235920.92385.2b.
Bessoud B, Denys A, Calmes JM, Madoff D, Qanadli S, Schnyder P, et al. Nonoperative management of traumatic splenic injuries: Is there a role for proximal splenic artery embolization? Am J Roentgenol 2006;186:779-85. https://doi.org/10.2214/AJR.04.1800.
Haan JM, Biffl W, Knudson MM, Davis KA, Oka T, Majercik S, et al. Splenic Embolization Revisited: A Multicenter Review. J Trauma - Inj Infect Crit Care 2004;56:542-7. https://doi.org/10.1097/01.TA.0000114069.73054.45.
Berg RJ, Inaba K, Okoye O, Pasley J, Teixeira PG, Esparza M, et al. The contemporary management of penetrating splenic injury. Injury 2014;45:1394-400. https://doi.org/10.1016/j.injury.2014.04.025.
Skattum J, Naess PA, Gaarder C. Non-operative management and immune function after splenic injury. Br J Surg 2012;99:59-65. https://doi.org/10.1002/bjs.7764.
Leone G, Pizzigallo E. Bacterial infections following splenectomy for malignant and nonmalignant hematologic diseases. Mediterr J Hematol Infect Dis 2015;7. https://doi.org/10.4084/MJHID.2015.057.
Lee HJ, Cheng CT, Chen CC, Liao CA, Chen SW, Wang SY, et al. Increased long-term pneumonia risk for the trauma-related splenectomized population - a population-based, propensity score matching study. Surg (United States) 2020;167:829-35. https://doi.org/10.1016/j.surg.2020.01.006.
Moore E, Cogbill T, Malangoni M, Jurkovich G, Champion H, Gennarelli T, et al. Organ injury scaling, II: pancreas, duodenum, small bowel, colon and rectum. J Trauma 1990;30:1427-9.
Copyright (c) 2021 Universidad del Valle

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0002-1641-0421
https://orcid.org/0000-0002-1641-0421


















