Damage control in penetrating duodenal trauma: less is better
Keywords:
Penetrating duodenal trauma, primary repair, duodenal reconstruction, primary anastomosis, damage control surgery, Injury Severity Score, Trauma Centers, Laparotomy, Retropneumoperitoneum, Pancreaticoduodenectomy, Jejunostomy, Gastric Bypass, Duodenum, Balloon OcclusionMain Article Content
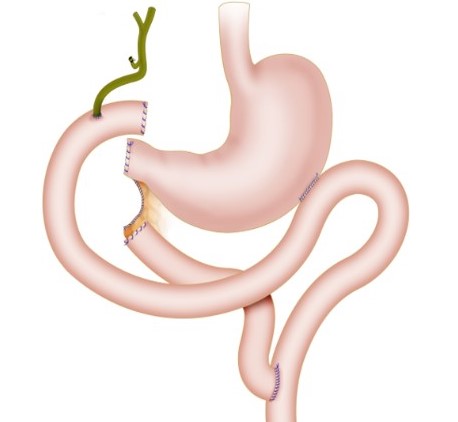
The overall incidence of duodenal injuries in severely injured trauma patients is between 0.2 to 0.6% and the overall prevalence in those suffering from abdominal trauma is 3 to 5%. Approximately 80% of these cases are secondary to penetrating trauma which are commonly associated with vascular and adjacent organ injuries. Therefore, defining the best surgical treatment algorithm remains controversial. Mild to moderate duodenal trauma is currently managed via primary repair and simple surgical techniques. However, severe injuries have required complex surgical techniques without significant favorable outcomes and consequential increase in the rates of mortality. The aim of this article is to delineate the experience in the surgical management of penetrating duodenal injuries via the creation of a practical and effective algorithm that includes basic principles of damage control surgery which sticks to the philosophy of “Less is Better”. Surgical management of all penetrating duodenal trauma should always default when possible to primary repair. When confronted with a complex duodenal injury, hemodynamic instability and/or significant associated injuries then the default should be damage control surgery. Definitive reconstructive surgery should be postponed until the patient has been adequately resuscitated and the diamond of death has been corrected.
Downloads

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-4495-7405
https://orcid.org/0000-0003-4495-7405