New clues to understand gastroschisis. Embryology, pathogenesis and epidemiology
Keywords:
Gastroschisis, abdominal abnormalities, Vitelline Duct, Ectopia Cordis, Genetic Predisposition to DiseaseMain Article Content
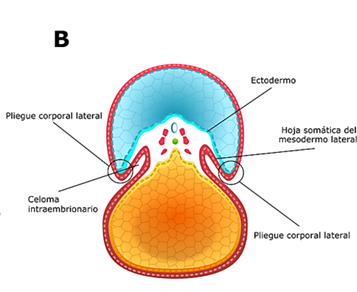
Gastroschisis is a congenital structural defect of the abdominal wall, most often to the right of the umbilicus, through which the abdominal viscera protrude. For a long time, its developmental, etiological, and epidemiological aspects have been a hot topic of controversy. However, recent findings suggest the involving of genetic and chromosomal alterations and the existence of a stress-inducing pathogenetic pathway, in which risk factors such as demographic and environmental ones can converge.
To expand the frontier of knowledge about a malformation that has shown a growing global prevalence, we have conducted a review of the medical literature that gathers information on the embryonic development of the ventral body wall, the primitive intestine and the ring-umbilical cord complex, as well as on the theories about its origin, pathogenesis and recent epidemiological evidence, for which we consulted bibliographic databases and standard search engines.
Downloads

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-0156-2577
https://orcid.org/0000-0003-0156-2577