Hemodynamically Unstable Pelvic Fracture: A Damage Control Surgical Algorithm that Fits your Reality
Keywords:
Hemodynamically Unstable, Damage Control, Pelvic Fracture, REBOA, Limited Resource CenterMain Article Content
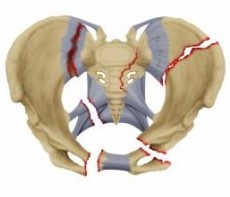
Pelvic fractures occur in up to 25% of all severely injured trauma patients and its mortality is markedly high despite advances in resuscitation and modernization of surgical techniques due to its inherent blood loss and associated extra-pelvic injuries. Pelvic ring volume increases significantly from fractures and/or ligament disruptions which precludes its inherent ability to self-tamponade resulting in accumulation of hemorrhage in the retroperitoneal space which inevitably leads to hemodynamic instability and the lethal diamond. Pelvic hemorrhage is mainly venous (80%) from the pre-sacral/pre-peritoneal plexus and the remaining 20% is of arterial origin (branches of the internal iliac artery). This reality can be altered via a sequential management approach that is tailored to the specific reality of the treating facility which involves a collaborative effort between orthopedic, trauma and intensive care surgeons. We propose two different management algorithms that specifically address the availability of qualified staff and existing infrastructure: one for the fully equipped trauma center and another for the very common limited resource center.
Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg 2017;12:1–18. https://doi.org/10.1186/s13017-017-0117-6.
Parry JA, Smith WR, Moore EE, Burlew CCC, Mauffrey C. The past, present, and future management of hemodynamic instability in patients with unstable pelvic ring injuries. Injury 2020. https://doi.org/10.1016/j.injury.2020.02.101.
Lewis RH, Sharpe JP, Berning B, Fabian TC, Croce MA, Magnotti LJ. Impact of a simplified management algorithm on outcome following exsanguinating pelvic fractures: A 10-year experience. J Trauma Acute Care Surg 2019;86:658–63. https://doi.org/10.1097/TA.0000000000002162.
Hernández L, Bru A. Fracturas Pélvicas: una visión moderna. Rev Española Cirugía Osteoartic 2015;50:39–48.
Lee HJ, No HK, Choi NJ, Sun HW, Lee JS, Jung YJ, et al. The size of pelvic hematoma can be a predictive factor for angioembolization in hemodynamically unstable pelvic trauma. Ann Surg Treat Res 2020;98:146–52. https://doi.org/10.4174/astr.2020.98.3.146.
Gordon WT, Fleming ME, Johnson AE, Gurney J, Shackelford S, Stockinger ZT. Pelvic fracture care. Mil Med 2018;183:115–7. https://doi.org/10.1093/milmed/usy111.
Manuel L, Núñez G. Trauma pélvico devastante. Cir Gen 2013;35:31–3.
Hermans E, Biert J, Edwards MJR. Epidemiology of Pelvic Ring Fractures in a Level 1 Trauma Center in the Netherlands. Hip Pelvis 2017;29:253. https://doi.org/10.5371/hp.2017.29.4.253.
Burlew CC, Moore EE, Stahel PF, Geddes AE, Wagenaar AE, Pieracci FM, et al. Preperitoneal pelvic packing reduces mortality in patients with life-threatening hemorrhage due to unstable pelvic fractures. J Trauma Acute Care Surg 2017;82:233–42. https://doi.org/10.1016/j.physbeh.2017.03.040.
Montmany S, Rebasa P, Luna A, Hidalgo JM, Cánovas G, Navarro S. Origen de la hemorragia en pacientes politraumatizados con fractura de pelvis e inestabilidad hemodinámica. Cir Esp 2015;93:450–4. https://doi.org/10.1016/j.ciresp.2015.01.011.
Guerra J, Posada Upegui JC, Giraldo Salazar OL. Morbimortalidad en trauma ortopédico de alta energía: estudio descriptivo retrospectivo. Rev Fac Nac Salud Pública 2018;36:28–36. https://doi.org/10.17533/udea.rfnsp.v36n2a05.
Martínez-Rondanelli A, Uribe JP, Escobar SS, Henao J, Ríos JA, Martínez-Cano JP. Control de daño y estabilización temprana definitiva en el tratamiento del paciente politraumatizado. Rev Colomb Ortop y Traumatol 2018;32:152–60. https://doi.org/10.1016/j.rccot.2017.11.009.
Advanced trauma life support (ATLS): 10th Edition. 2018. https://doi.org/10.1111/j.1365-2044.1993.tb07026.x.
Pape HC, Peitzman AB, Rotondo MF, Giannoudis PV. Damage Control Management in the Polytrauma Patient. 2018.
Moore EE, Feliciano D V, Mattox KL. Trauma. 2017.
Alton TB, Gee AO. Classifications in brief: Young and Burgess classification of pelvic ring injuries. Clin Orthop Relat Res 2014;472:2338–42. https://doi.org/10.1007/s11999-014-3693-8.
Ordoñez CA, Herrera-Escobar JP, Parra MW, Rodriguez-Ossa PA, Mejia DA, Sanchez AI, et al. Computed tomography in hemodynamically unstable severely injured blunt and penetrating trauma patients. J. Trauma Acute Care Surg., vol. 80, Lippincott Williams and Wilkins; 2016, p. 597–603. https://doi.org/10.1097/TA.0000000000000975.
Burlew CC, Moore EE, Smith WR, Johnson JL, Biffl WL, Barnett CC, et al. Preperitoneal pelvic packing/external fixation with secondary angioembolization: Optimal care for life-threatening hemorrhage from unstable pelvic fractures. J Am Coll Surg 2011;212:628–35. https://doi.org/10.1016/j.jamcollsurg.2010.12.020.
Papakostidis C, Kanakaris N, Dimitriou R, Giannoudis P V. The role of arterial embolization in controlling pelvic fracture haemorrhage: A systematic review of the literature. Eur J Radiol 2012;81:897–904. https://doi.org/10.1016/j.ejrad.2011.02.049.
Croce MA, Magnotti LJ, Savage SA, Wood GW, Fabian TC. Emergent Pelvic Fixation in Patients with Exsanguinating Pelvic Fractures. J Am Coll Surg 2007;204:935–9. https://doi.org/10.1016/j.jamcollsurg.2007.01.059.
Fraser J, Cowell WM. Clinical study of blood pressure in wound conditions. Nat Treat Wound Shock Allied Cond 1917;70:520–35.
Cannon JW, Khan MA, Raja AS, Cohen MJ, Como JJ, Cotton BA, et al. Damage control resuscitation in patients with severe traumatic hemorrhage: A practice management guideline from the Eastern Association for the Surgery of Trauma. J. Trauma Acute Care Surg., vol. 82, Lippincott Williams and Wilkins; 2017, p. 605–17. https://doi.org/10.1097/TA.0000000000001333.
Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: The PROPPR randomized clinical trial. JAMA - J Am Med Assoc 2015;313:471–82. https://doi.org/10.1001/jama.2015.12.
Ordoñez CA, Pino LF, Badiel M, Sánchez AI, Loaiza J, Ballestas L, et al. Safety of performing a delayed anastomosis during damage control laparotomy in patients with destructive colon injuries. J. Trauma - Inj. Infect. Crit. Care, vol. 71, 2011, p. 1512–8. https://doi.org/10.1097/TA.0b013e31823d0691.
Egea-Guerrero JJ, Freire-Aragón MD, Serrano-Lázaro A, Quintana-Díaz M. Objetivos y nuevas estrategias de resucitación en el paciente traumatizado grave. Med Intensiva 2014;38:502–12. https://doi.org/10.1016/j.medin.2014.06.003.
Toth L, King KL, McGrath B, Balogh ZJ. Efficacy and safety of emergency non-invasive pelvic ring stabilisation. Injury 2012;43:1330–4. https://doi.org/10.1016/j.injury.2012.05.014.
Jowett AJL, Bowyer GW. Pressure characteristics of pelvic binders. Injury 2007;38:118–21. https://doi.org/10.1016/j.injury.2006.03.018.
Stahel PF, Burlew CC, Moore EE. Current trends in the management of hemodynamically unstable pelvic ring injuries. Curr Opin Crit Care 2017;23:511–9. https://doi.org/10.1097/MCC.0000000000000454.
Smith WR, Moore EE, Osborn P, Agudelo JF, Morgan SJ, Parekh AA, et al. Retroperitoneal packing as a resuscitation technique for hemodynamically unstable patients with pelvic fractures: Report of two representative cases and a description of technique. J Trauma - Inj Infect Crit Care 2005;59:1510–4. https://doi.org/10.1097/01.ta.0000197330.81352.94.
Abrassart S, Stern R, Peter R. Unstable pelvic ring injury with hemodynamic instability: What seems the best procedure choice and sequence in the initial management? Orthop Traumatol Surg Res 2013;99:175–82. https://doi.org/10.1016/j.otsr.2012.12.014.
Li Q, Dong J, Yang Y, Wang G, Wang Y, Liu P, et al. Retroperitoneal packing or angioembolization for haemorrhage control of pelvic fractures - Quasi-randomized clinical trial of 56 haemodynamically unstable patients with Injury Severity Score ≥33. Injury 2016;47:395–401. https://doi.org/10.1016/j.injury.2015.10.008.
Chiara O, di Fratta E, Mariani A, Michaela B, Prestini L, Sammartano F, et al. Efficacy of extra-peritoneal pelvic packing in hemodynamically unstable pelvic fractures, a Propensity Score Analysis. World J Emerg Surg 2016;11:1–8. https://doi.org/10.1186/s13017-016-0077-2.
Monchal T, Hornez E, Coisy M, Bourgouin S, de Roulhac J, Balandraud P. Preperitoneal pelvic packing. J Visc Surg 2017;154:S57–60. https://doi.org/10.1016/j.jviscsurg.2017.08.006.
Filiberto DM, Fox AD. Preperitoneal pelvic packing: Technique and outcomes. Int J Surg 2016;33:222–4. https://doi.org/10.1016/j.ijsu.2016.05.072.
Tang J, Shi Z, Hu J, Wu H, Yang C, Le G, et al. Optimal sequence of surgical procedures for hemodynamically unstable patients with pelvic fracture: A network meta-analysis. Am J Emerg Med 2019;37:571–8. https://doi.org/10.1016/j.ajem.2018.06.027.
Suzuki T, Smith WR, Moore EE. Pelvic packing or angiography: Competitive or complementary? Injury 2009;40:343–53. https://doi.org/10.1016/j.injury.2008.12.006.
Osborn PM, Smith WR, Moore EE, Cothren CC, Morgan SJ, Williams AE, et al. Direct retroperitoneal pelvic packing versus pelvic angiography: A comparison of two management protocols for haemodynamically unstable pelvic fractures. Injury 2009;40:54–60. https://doi.org/10.1016/j.injury.2008.08.038.
Tai DKC, Li WH, Lee KY, Cheng M, Lee KB, Tang LF, et al. Retroperitoneal pelvic packing in the management of hemodynamically unstable pelvic fractures: A level I trauma center experience. J Trauma 2011;71:E79–86. https://doi.org/10.1097/TA.0b013e31820cede0.
Halawi MJ. Pelvic ring injuries: Emergency assessment and management. J Clin Orthop Trauma 2015;6:252–8. https://doi.org/10.1016/j.jcot.2015.08.002.
Ordoñez CA, Manzano-Nunez R, del Valle AM, Rodriguez F, Burbano P, Naranjo MP, et al. Uso actual del balón de resucitación aórtico endovascular (REBOA) en trauma. Rev Colomb Anestesiol 2017;45:30–8. https://doi.org/10.1016/j.rca.2017.07.012.
Coccolini F, Ceresoli M, McGreevy DT, Sadeghi M, Pirouzram A, Toivola A, et al. Aortic balloon occlusion (REBOA) in pelvic ring injuries: preliminary results of the ABO Trauma Registry. Updates Surg 2020. https://doi.org/10.1007/s13304-020-00735-4.
Jarvis S, Kelly M, Mains C, Corrigan C, Patel N, Carrick M, et al. A descriptive survey on the use of resuscitative endovascular balloon occlusion of the aorta (REBOA) for pelvic fractures at US level I trauma centers. Patient Saf Surg 2019;13:1–9. https://doi.org/10.1186/s13037-019-0223-3.
Downloads

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0003-0617-4303
https://orcid.org/0000-0003-0617-4303