Reinterventions after damage control surgery
Keywords:
Laparotomy, Ostomy, Thoracic Cavity, Anastomosis, Surgical, Postoperative Period, Cardiac Surgical Procedures, Intensive Care Units, Surgical Wound Infection, Colostomy, Abdominal Wall, Reoperation, Intra-Abdominal HypertensionMain Article Content
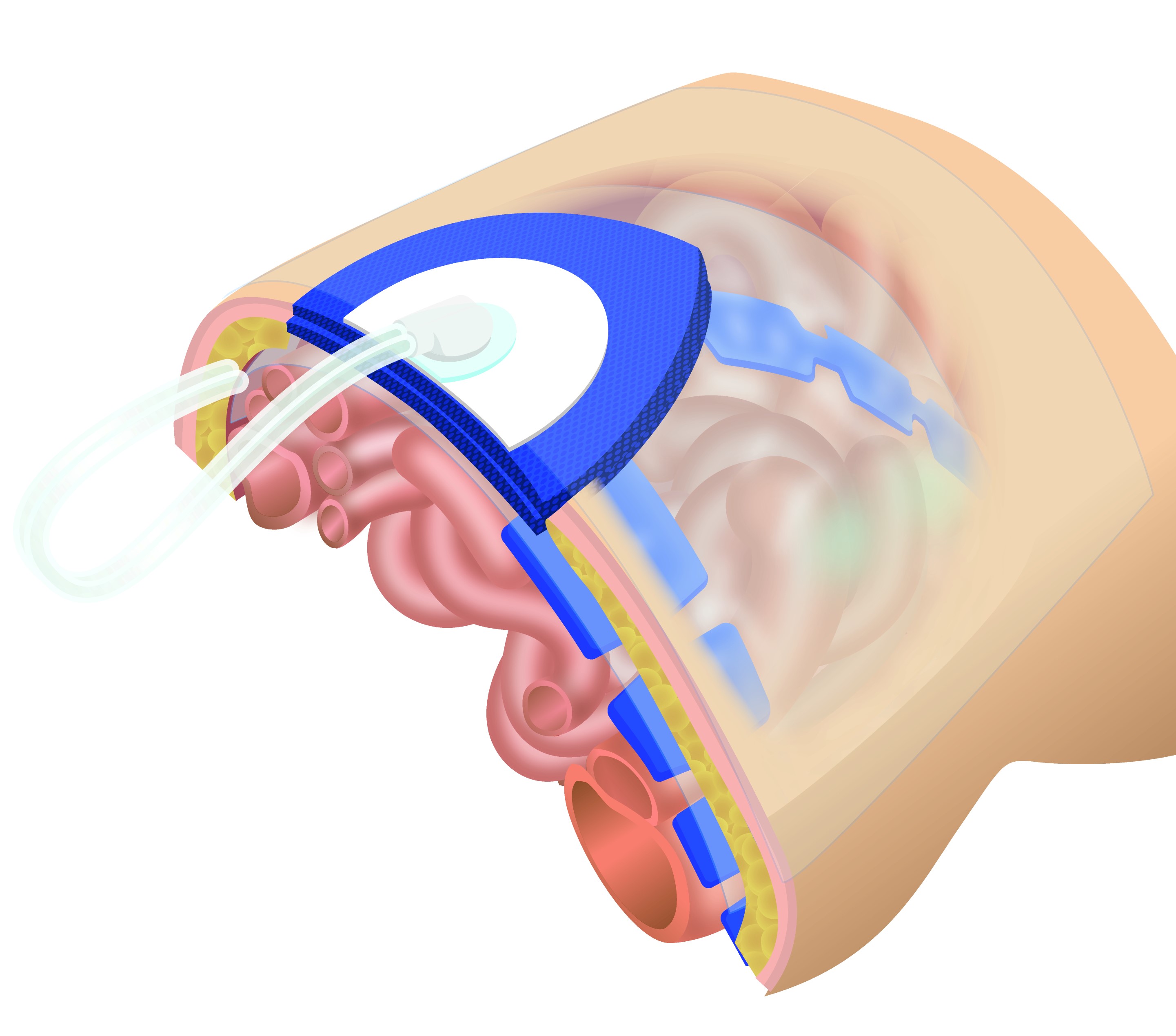
Damage control has well-defined steps. However, there are still controversies regarding whom, when, and how re-interventions should be performed. This article summarizes the Trauma and Emergency Surgery Group (CTE) Cali-Colombia recommendations about the specific situations concerning second interventions of patients undergoing damage control surgery. We suggest packing as the preferred bleeding control strategy, followed by unpacking within the next 48-72 hours. In addition, a deferred anastomosis is recommended for correction of intestinal lesions, and patients treated with vascular shunts should be re-intervened within 24 hours for definitive management. Furthermore, abdominal or thoracic wall closure should be attempted within eight days. These strategies aim to decrease complications, morbidity, and mortality.
Downloads

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0002-5326-2317
https://orcid.org/0000-0002-5326-2317