Recurrent acute coronary syndrome after infliximab infusion in a patient with rheumatoid arthritis Case report
Keywords:
Rheumatoid arthritis, Myocardial ischemia, Infliximab, Biological Products, Tumor Necrosis Factor Inhibitors, Adverse drug reactionsMain Article Content
Case description:
A 61-year-old male patient with uncontrolled rheumatoid arthritis presented acute coronary syndrome three times less than 48 hours after infliximab infusion.
Clinical findings:
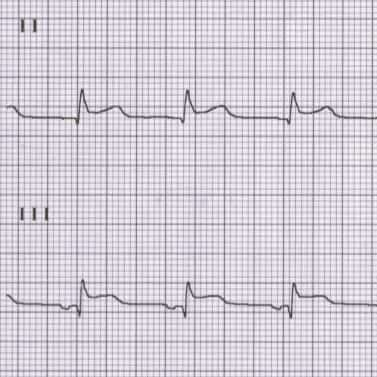
He presented with ST-elevation myocardial infarction on two occasions and nonST-elevation acute coronary syndrome on one, with the identification of multivessel coronary disease.
Treatment and outcome:
The coronary intervention was performed with thrombus aspiration, medicated stent implantation, medicated balloon angioplasty, discontinuation of infliximab, and modification and optimization of cardiovascular pharmacological management.
Clinical relevance:
Patients with rheumatoid arthritis have subclinical cardiovascular disease and increased cardiovascular risk. The evidence regarding the relationship between infliximab and ischemic heart disease is controversial. A broad clinical spectrum of cardiac involvement with infliximab infusion is found in case reports, ranging from stable angina to ST-segment elevation acute coronary syndrome. The pathophysiology is not elucidated, with hypotheses proposing plaque rupture, allergic reactions, and vasoconstriction as possible disease mechanisms. The direct association between infliximab infusion and acute coronary syndrome needs more clinical research to optimize the management and prognosis of patients with this type of complication.
Aletaha D, Smolen JS. Diagnosis and Management of Rheumatoid Arthritis: A Review. JAMA. 2018;320(13):1360-1372. doi:10.1001/JAMA.2018.13103 DOI: https://doi.org/10.1001/jama.2018.13103
Fernández-Ávila DG, Rincón-Riaño DN, Bernal-Macías S, et al. Prevalencia de la artritis reumatoide en Colombia según información del Sistema Integral de Información de la Protección Social. Revista Colombiana de Reumatología. 2019;26(2):83-87. doi:10.1016/J.RCREU.2019.01.003 DOI: https://doi.org/10.1016/j.rcreu.2019.01.003
Widdifield J, Paterson JM, Huang A, Bernatsky S. Causes of Death in Rheumatoid Arthritis: How Do They Compare to the General Population? Arthritis Care Res (Hoboken). 2018;70(12):1748-1755. doi:10.1002/ACR.23548 DOI: https://doi.org/10.1002/acr.23548
Jagpal A, Navarro-Millán I. Cardiovascular co-morbidity in patients with rheumatoid arthritis: a narrative review of risk factors, cardiovascular risk assessment and treatment. BMC Rheumatology 2018 2:1. 2018;2(1):1-14. doi:10.1186/S41927-018-0014-Y DOI: https://doi.org/10.1186/s41927-018-0014-y
Klotz U, Teml A, Schwab M. Clinical Pharmacokinetics and Use of Infliximab. Clinical Pharmacokinetics 2007 46:8. 2012;46(8):645-660. doi:10.2165/00003088-200746080-00002 DOI: https://doi.org/10.2165/00003088-200746080-00002
Smolen JS, Landewé RBM, Bijlsma JWJ, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2019 update. Ann Rheum Dis. 2020;79(6):685-699. doi:10.1136/ANNRHEUMDIS-2019-216655 DOI: https://doi.org/10.1136/annrheumdis-2019-216655
Woodrick RS, Ruderman EM. Safety of biologic therapy in rheumatoid arthritis. Nat Rev Rheumatol. 2011;7(11):639-652. doi:10.1038/NRRHEUM.2011.145 DOI: https://doi.org/10.1038/nrrheum.2011.145
Janssen Biotech Inc. 2020. REMICADE (Infliximab). U.S. Food and Drug Administration website. www.accessdata.fda.gov/drugsatfda_docs/label/2013/103772s5359lbl.pdf. Accessed May 14, 2022. https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/103772s5359lbl.pdf
Delcoigne B, Ljung L, Provan SA, et al. Short-term, intermediate-term and long-term risks of acute coronary syndrome in cohorts of patients with RA starting biologic DMARDs: results from four Nordic countries. Ann Rheum Dis. 2022;0:annrheumdis-2021-221996. doi:10.1136/ANNRHEUMDIS-2021-221996 DOI: https://doi.org/10.1136/annrheumdis-2021-221996
Low ASL, Symmons DPM, Lunt M, et al. Relationship between exposure to tumour necrosis factor inhibitor therapy and incidence and severity of myocardial infarction in patients with rheumatoid arthritis. Ann Rheum Dis. 2017;76(4):654-660. doi:10.1136/ANNRHEUMDIS-2016-209784 DOI: https://doi.org/10.1136/annrheumdis-2016-209784
Zhang J, Xie F, Yun H, et al. Comparative effects of biologics on cardiovascular risk among older patients with rheumatoid arthritis. Ann Rheum Dis. 2016;75(10):1813-1818. doi:10.1136/ANNRHEUMDIS-2015-207870 DOI: https://doi.org/10.1136/annrheumdis-2015-207870
Settergren M, Tornvall P. Does TNF-alpha blockade cause plaque rupture? Atherosclerosis. 2004;173(1):149. doi:10.1016/J.ATHEROSCLEROSIS.2003.12.009 DOI: https://doi.org/10.1016/j.atherosclerosis.2003.12.009
Abedin M, Scheurich D, Reimold SC, Reimold AM. Acute coronary syndrome after infliximab infusion. Cardiol Rev. 2006;14(1):50-52. doi:10.1097/01.CRD.0000178320.51474.AC DOI: https://doi.org/10.1097/01.crd.0000178320.51474.ac
Casallo Blanco S, Aragón Díez A, Marcos Sánchez F, Cantalejo Moreira MA, Joya Seijo D, Vicente Martín C. [Infliximab and acute myocardial infarction]. An Med Interna. 2005;22(6):301-302. doi:10.4321/S0212-71992005000600015 DOI: https://doi.org/10.4321/S0212-71992005000600015
Panteris V, Perdiou A, Tsirimpis V, Karamanolis DG. Acute coronary syndrome after infliximab therapy in a patient with Crohn’s disease. World J Gastroenterol. 2006;12(38):6235-6238. doi:10.3748/wjg.v12.i38.6235 DOI: https://doi.org/10.3748/wjg.v12.i38.6235
Kumar A, Ghose T, Mendiratta N, Prajapati PK, Abrol A. Acute coronary syndrome caused by infliximab in a patient with ankylosing spondylitis. Int J Rheum Dis. 2013;16(2):235-236. doi:10.1111/1756-185X.12052 DOI: https://doi.org/10.1111/1756-185X.12052
Sivasubramanian N, Coker ML, Kurrelmeyer KM, et al. Left ventricular remodeling in transgenic mice with cardiac restricted overexpression of tumor necrosis factor. Circulation. 2001;104(7):826-831. doi:10.1161/HC3401.093154 DOI: https://doi.org/10.1161/hc3401.093154
Kotani T, Takeuchi T, Takai S, et al. Serum levels of matrix metalloproteinase (MMP) 9, a risk factor for acute coronary syndrome, are reduced independently of serum MMP-3 by anti-TNF-α antibody (infliximab) therapy in patients with rheumatoid arthritis. J Pharmacol Sci. 2012;120(1):50-53. doi:10.1254/JPHS.12129SC DOI: https://doi.org/10.1254/jphs.12129SC
Kounis NG, Kounis GN, Soufras GD, Tsigkas G, Hahalis G. Attention to Infliximab adverse events: chimeric monoclonal antibodies can induce anti chimeric antibodies that may result in Kounis hypersensitivity associated acute coronary syndrome. Eur Rev Med Pharmacol Sci. 2014;18(24):3735-3736. Accessed May 14, 2022. https://pubmed.ncbi.nlm.nih.gov/25555859/
Bălănescu A, Bojincă V, Bojincă M, Donisan T, Bălănescu S. Cardiovascular effects of methotrexate in immune-mediated inflammatory diseases. Exp Ther Med. 2019;17(2). doi:10.3892/ETM.2018.6992 DOI: https://doi.org/10.3892/etm.2018.6992
van Ede AE, Laan RFJM, Blom HJ, et al. Homocysteine and folate status in methotrexate-treated patients with rheumatoid arthritis. Rheumatology (Oxford). 2002;41(6):658-665. doi:10.1093/RHEUMATOLOGY/41.6.658 DOI: https://doi.org/10.1093/rheumatology/41.6.658
Bajic Z, Sobot T, Skrbic R, et al. Homocysteine, Vitamins B6 and Folic Acid in Experimental Models of Myocardial Infarction and Heart Failure—How Strong Is That Link? Biomolecules 2022, Vol 12, Page 536. 2022;12(4):536. doi:10.3390/BIOM12040536 DOI: https://doi.org/10.3390/biom12040536
Yan J, Zhou J, Huang J, Zhang H, Deng Z, Du Y. The outcomes of acute myocardial infarction patients comorbidity with hypertension and hyperhomocysteinemia. Scientific Reports 2021 11:1. 2021;11(1):1-7. doi:10.1038/s41598-021-02340-w DOI: https://doi.org/10.1038/s41598-021-02340-w
Lin JS, Evans C v., Johnson E, Redmond N, Coppola EL, Smith N. Nontraditional Risk Factors in Cardiovascular Disease Risk Assessment: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2018;320(3):281-297. doi:10.1001/JAMA.2018.4242 DOI: https://doi.org/10.1001/jama.2018.4242
Whayne TF. Non-Traditional Cardiovascular Risk Markers in the Era of Established Major Risk Factors and Multiple Guidelines. Curr Vasc Pharmacol. 2018;17(3):270-277. doi:10.2174/1570161116666180123112956 DOI: https://doi.org/10.2174/1570161116666180123112956
Downloads

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0000-0002-4189-4317
https://orcid.org/0000-0002-4189-4317