JAK2, CALR, and MPL Mutation Profiles in Colombian patients with BCR-ABL Negative Myeloproliferative Neoplasms
Keywords:
Thrombocythemia, Essential, Primary Myelofibrosis, Polycythemia Vera, Myeloproliferative Disorders, Janus Kinase 2, STAT Transcription FactorsMain Article Content
Background
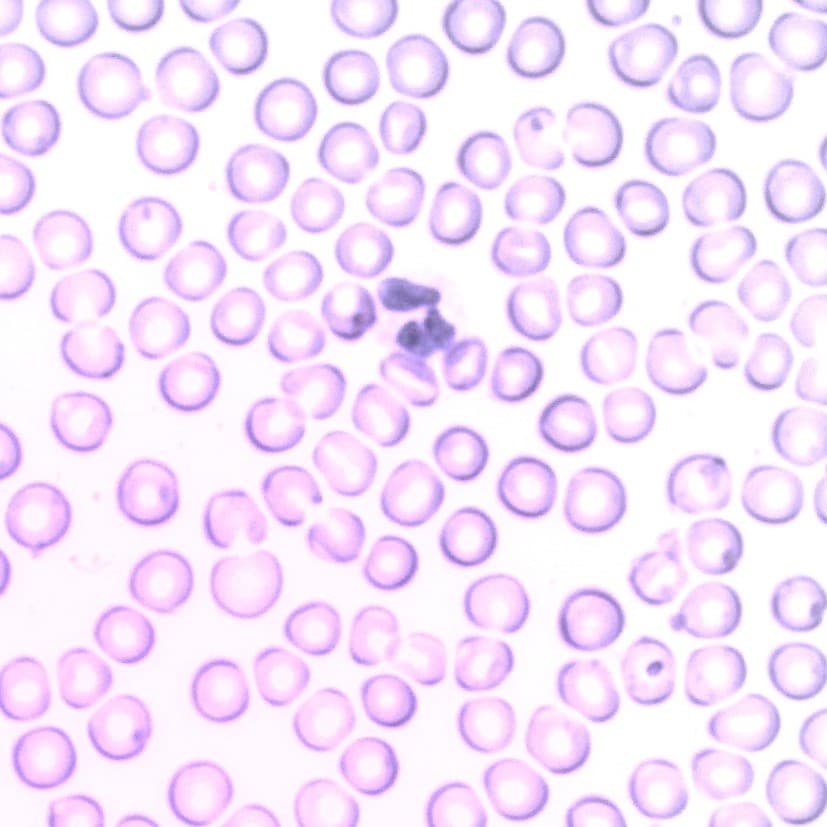
Among the chronic myeloproliferative neoplasms (MPNs) not associated with BCR-ABL mutations are polycythemia vera, primary myelofibrosis, and essential thrombocythemia. These diseases are caused by gene mutations, such as the JAK2, MPL, and CALR genes, which regulate the JAK-STAT signaling pathway.
Objective
This study aimed to establish the frequencies of mutations in the JAK2, MPL, and CALR genes in Colombian patients with a negative clinical diagnosis of BCR-ABL chronic myeloproliferative neoplasms.
Methods
The JAK2 V617F and MPL W515K mutations and deletions or insertions in exon 9 of the CALR gene were analyzed in 52 Colombian patients with polycythemia vera, primary myelofibrosis, and essential thrombocythemia.
Results
The JAK2V617F mutation was carried by 51.9% of the patients, the CALR mutation by 23%, and the MPL mutation by 3.8%; 23% were triple-negative for the mutations analyzed. Six mutation types in CALR were identified in these neoplasms, one of which has not been previously reported. Additionally, one patient presented a double mutation in the CALR and JAK2 genes. Regarding the hematological results for the mutations, significant differences were found in the hemoglobin level, hematocrit level, and platelet count among the three neoplasms.
Conclusion
Thus, this study demonstrates the importance of the molecular characterization of the JAK2, CALR and MPL mutations in Colombian patients (the genetic context of which remains unclear in the abovementioned neoplasms) to achieve an accurate diagnosis, a good prognosis, adequate management, and patient survival.
Nann D, Fend F. Synoptic diagnostics of myeloproliferative neoplasms: Morphology and molecular genetics. Cancers. 2021;13(14):1-22. https://doi.org/10.3390/cancers13143528 PMid:34298741 PMCid:PMC8303289 DOI: https://doi.org/10.3390/cancers13143528
Shallis RM, Zeidan AM, Wang R, Podoltsev NA. Epidemiology of the Philadelphia Chromosome-Negative Classical Myeloproliferative Neoplasms. Hematology/Oncology Clinics of North America. 2021;35(2):177-89. https://doi.org/10.1016/j.hoc.2020.11.005 PMid:33641862 DOI: https://doi.org/10.1016/j.hoc.2020.11.005
Abello V, Quintero G, Espinosa D, Solano MH, Casas CP, Saavedra D, et al. Descripción de las características clínicas de las neoplasias mieloproliferativas crónicas ( NMPC ) Description of the clinical characteristics of chronic myeloproliferative neoplasms ( MPNs ) First report of the colombian registry of MPNs. Acta Médica Colombiana. 2017;42(1):35-41. https://doi.org/10.36104/amc.2017.624 DOI: https://doi.org/10.36104/amc.2017.624
Langabeer SE, Andrikovics H, Asp J, Bellosillo B, Carillo S, Haslam K, et al. Molecular diagnostics of myeloproliferative neoplasms. European J Haematol. 2015;95(4):270-9. https://doi.org/10.1111/ejh.12578 PMid:25951317 DOI: https://doi.org/10.1111/ejh.12578
Ferreira Cristina S, Polo B, Lacerda JF. Somatic Mutations in Philadelphia Chromosome-Negative Myeloproliferative Neoplasms. Seminars in Hematology. 2018;55(4):215-22. https://doi.org/10.1053/j.seminhematol.2018.04.005 PMid:30502850 DOI: https://doi.org/10.1053/j.seminhematol.2018.04.005
Araki M, Komatsu N. The role of calreticulin mutations in myeloproliferative neoplasms. International Journal of Hematology. 2020;111(2):200-5. https://doi.org/10.1007/s12185-019-02800-0 PMid:31848992 DOI: https://doi.org/10.1007/s12185-019-02800-0
Vainchenker W, Dusa A, Constantinescu SN. JAKs in pathology: Role of Janus kinases in hematopoietic malignancies and immunodeficiencies. Seminars in Cell and Developmental Biology. 2008;19(4):385-93. https://doi.org/10.1016/j.semcdb.2008.07.002 PMid:18682296 DOI: https://doi.org/10.1016/j.semcdb.2008.07.002
Song J, Hussaini M, Zhang H, Shao H, Qin D, Zhang X, et al. Comparison of the Mutational Profiles of Primary Myelofibrosis, Polycythemia Vera, and Essential Thrombocytosis. American Journal of Clinical Pathology. 2017;147(5):444-52. https://doi.org/10.1093/ajcp/aqw222 PMid:28419183 PMCid:PMC5402718 DOI: https://doi.org/10.1093/ajcp/aqw222
Tefferi A, Pardanani A. Myeloproliferative neoplasms: A contemporary review. JAMA Oncology. 2015;1(1):97-105. https://doi.org/10.1001/jamaoncol.2015.89 PMid:26182311 DOI: https://doi.org/10.1001/jamaoncol.2015.89
Brown NA, Elenitoba-Johnson KSJ. Update from the 4th Edition of the World Health Organization Classification of Head and Neck Tumours: Hematolymphoid Tumours. Head and Neck Pathology. 2017;11(1):96-109. https://doi.org/10.1007/s12105-017-0802-5 PMid:28247223 PMCid:PMC5340738 DOI: https://doi.org/10.1007/s12105-017-0802-5
Furtado LV, Weigelin HC, Elenitoba-Johnson KSJ, Betz BL. A Multiplexed fragment analysis-based assay for detection of JAK2 exon 12 mutations. Journal of Molecular Diagnostics. 2013;15(5):592-9. https://doi.org/10.1016/j.jmoldx.2013.04.006 PMid:23810504 DOI: https://doi.org/10.1016/j.jmoldx.2013.04.006
Jones AV, Ward D, Lyon M, Leung W, Callaway A, Chase A, et al. Evaluation of methods to detect CALR mutations in myeloproliferative neoplasms. Leukemia Research. 2015;39(1):82-7. https://doi.org/10.1016/j.leukres.2014.11.019 PMid:25499808 DOI: https://doi.org/10.1016/j.leukres.2014.11.019
Klampfl T, Gisslinger H, Harutyunyan AS, Nivarthi H, Rumi E, Milosevic JD, et al. Somatic Mutations of Calreticulin in Myeloproliferative Neoplasms. New England Journal of Medicine. 2013;369(25):2379-90. https://doi.org/10.1056/NEJMoa1311347 PMid:24325356 DOI: https://doi.org/10.1056/NEJMoa1311347
R Core Team (2017). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. https://www.R-project.org/.
Ojeda MJ, Bragós IM, Calvo KL, Williams GM, Carbonell MM, Pratti AF. CALR, JAK2 and MPL mutation status in Argentinean patients with BCR-ABL1- negative myeloproliferative neoplasms. Hematology. 2018; 23(4):208-11. https://doi.org/10.1080/10245332.2017.1385891 PMid:28990497 DOI: https://doi.org/10.1080/10245332.2017.1385891
Labastida-Mercado N, Galindo-Becerra S, Garcés-Eisele J, Colunga-Pedraza P, Guzman-Olvera V, Reyes-Nuñez V, et al. The mutation profile of JAK2, MPL and CALR in Mexican patients with Philadelphia chromosome-negative myeloproliferative neoplasms. Hematology/ Oncology and Stem Cell Therapy. 2015;8(1):16-21. https://doi.org/10.1016/j.hemonc.2014.12.002 PMid:25637689 DOI: https://doi.org/10.1016/j.hemonc.2014.12.002
Kim SY, Im K, Park SN, Kwon J, Kim JA, Lee DS. CALR, JAK2, and MPL mutation profiles in patients with four different subtypes of myeloproliferative neoplasms: Primary myelofibrosis, essential thrombocythemia, polycythemia vera, and myeloproliferative neoplasm, unclassifiable. American Journal of Clinical Pathology. 2015;143(5):635-44. https://doi.org/10.30699/ijp.2021.136458.2495 PMid:33936230 PMCid:PMC8085288 DOI: https://doi.org/10.1309/AJCPUAAC16LIWZMM
Szuber N, Mudireddy M, Nicolosi M, Penna D, Vallapureddy R, Lasho TL, et al. 3,023 Mayo Clinic Patients with Myeloproliferative Neoplasms: Risk-Stratified Comparison of Survival and Outcomes Data Among Disease Subgroups. Blood. 2018;132(Supplement 1):3035-3035. https://doi.org/10.1016/j.mayocp.2018.08.022 PMid:30824279 DOI: https://doi.org/10.1182/blood-2018-99-109740
Misawa K, Yasuda H, Araki M, Ochiai T, Morishita S, Shirane S, et al. Mutational subtypes of JAK2 and CALR correlate with different clinical features in Japanese patients with myeloproliferative neoplasms. International Journal of Hematology. 2018;107(6):673-80. https://doi.org/10.1007/s12185-018-2421-7 PMid:29464483 DOI: https://doi.org/10.1007/s12185-018-2421-7
Pietra D, Rumi E, Ferretti V V., Di Buduo CA, Milanesi C, Cavalloni C, et al. Differential clinical effects of different mutation subtypes in CALR-mutant myeloproliferative neoplasms. Leukemia. 2016;30(2):431-8. DOI: 10.1038/leu.2015.277 https://doi.org/10.1038/leu.2015.277 PMid:26449662 PMCid:PMC4740452 DOI: https://doi.org/10.1038/leu.2015.277
Machado-Neto JA, de Melo Campos P, de Albuquerque DM, Costa FF, Lorand-Metze I, Olalla Saad ST, et al. Somatic mutations of calreticulin in a Brazilian cohort of patients with myeloproliferative neoplasms. Revista Brasileira de Hematologia e Hemoterapia. 2015;37(3):211-4. https://doi.org/10.1016/j.bjhh.2015.03.012 PMid:26041426 PMCid:PMC4459485 DOI: https://doi.org/10.1016/j.bjhh.2015.03.012
Singdong R, Siriboonpiputtana T, Chareonsirisuthigul T, Kongruang A, Limsuwanachot N, Sirirat T, et al. Characterization and Prognosis Significance of JAK2 (V617F), MPL, and CALR Mutations in PhiladelphiaNegative Myeloproliferative Neoplasms. Asian Pacific Journal of Cancer Prevention. 2016;17(10):4647-53. https://doi.org/10.22034/APJCP.2016.17.10.4647
Lang T, Nie Y, Wang Z, Huang Q, An L, Wang Y, et al. Correlation analysis between JAK2, MPL, and CALR mutations in patients with myeloproliferative neoplasms of Chinese Uygur and Han nationality and their clinical characteristics. Journal of International Medical Research. 2018;46(11):4650-9. https://doi.org/10.1177/0300060518787719 PMid:30084272 PMCid:PMC6259388 DOI: https://doi.org/10.1177/0300060518787719
Rabade N, Subramanian PG, Kodgule R, Raval G, Joshi S, Chaudhary S, et al. Molecular genetics of BCR-ABL1 negative myeloproliferative neoplasms in India. Indian Journal of Pathology and Microbiology. 2018;61(2):209-13. https://doi.org/10.4103/IJPM.IJPM_223_17 PMid:29676359 DOI: https://doi.org/10.4103/IJPM.IJPM_223_17
Nunes DPT, de Lima LT, Chauffaille M de L, Mitne-Neto M, dos Santos MT, Cliquet MG, et al. CALR mutations screening in wild type JAK2V617F and MPLW515K/L Brazilian myeloproliferative neoplasm patients. Blood Cells, Molecules, and Diseases. 2015;55(3):236-40. https://doi.org/10.1016/j.bcmd.2015.07.005 PMid:26227853 DOI: https://doi.org/10.1016/j.bcmd.2015.07.005
Soliman EA, El-Ghlban S, El-Aziz SA, Abdelaleem A, Shamaa S, Abdel-Ghaffar H. JAK2, CALR, and MPL Mutations in Egyptian Patients With Classic Philadelphia-negative Myeloproliferative Neoplasms. Clinical Lymphoma, Myeloma and Leukemia. 2020;20(10):e645-51. https://doi.org/10.1016/j.clml.2020.05.011 PMid:32591258 DOI: https://doi.org/10.1016/j.clml.2020.05.011
Vainchenker W, Kralovics R. Genetic basis and molecular pathophysiology of classical myeloproliferative neoplasms. Blood. 2017;129(6):667-79. https://doi.org/10.1182/blood-2016-10-695940 PMid:28028029 DOI: https://doi.org/10.1182/blood-2016-10-695940
Pardanani AD, Levine RL, Lasho T, Pikman Y, Mesa RA, Wadleigh M, et al. MPL515 mutations in myeloproliferative and other myeloid disorders: A study of 1182 patients. Blood. 2006;108(10):3472-6. https://doi.org/10.1182/blood-2006-04-018879 PMid:16868251 DOI: https://doi.org/10.1182/blood-2006-04-018879
Lundberg P, Karow A, Nienhold R, Looser R, Hao-Shen H, Nissen I, et al. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood. 2014;123(14):2220-8. https://doi.org/10.1182/blood-2013-11-537167 PMid:24478400 DOI: https://doi.org/10.1182/blood-2013-11-537167
Mcgaffin G, Harper K, Stirling D, Mclintock L. JAK2 V617F and CALR mutations are not mutually exclusive; findings from retrospective analysis of a small patient cohort. British Journal of Haematology. 2014;167(2):276-8. https://doi.org/10.1111/bjh.12969 PMid:24935260 DOI: https://doi.org/10.1111/bjh.12969
Jeong JH, Lee HT, Seo JY, Seo YH, Kim KH, Kim MJ, et al. Screening PCR versus sanger sequencing:Detection of CALR mutations in patients with thrombocytosis. Annals of Laboratory Medicine. 2016;36(4):291-9. https://doi.org/10.3343/alm.2016.36.4.291 PMid:27139600 PMCid:PMC4855047 DOI: https://doi.org/10.3343/alm.2016.36.4.291
Chen CC, Gau JP, Chou HJ, You JY, Huang CE, Chen YY, et al. Frequencies, clinical characteristics, and outcome of somatic CALR mutations in JAK2-unmutated essential thrombocythemia. Annals of Hematology. 2014;93(12):2029-36. https://doi.org/10.1007/s00277-014-2151-8 PMid:25015052 DOI: https://doi.org/10.1007/s00277-014-2151-8
Tefferi A, Lasho TL, Finke CM, Knudson RA, Ketterling R, Hanson CH, et al. CALR vs JAK2 vs MPLmutated or triple-negative myelofibrosis: Clinical, cytogenetic and molecular comparisons. Leukemia. 2014;28(7):1472-7. https://doi.org/10.1038/leu.2014.3 PMid:24402162 DOI: https://doi.org/10.1038/leu.2014.3
Tefferi A, Wassie EA, Guglielmelli P, Gangat N, Belachew AA, Lasho TL, et al. Type 1 versus Type 2 calreticulin mutations in essential thrombocythemia: A collaborative study of 1027 patients. American Journal of Hematology. 2014;89(8):121-4. https://doi.org/10.1002/ajh.23743 DOI: https://doi.org/10.1002/ajh.23743
Shirane S, Araki M, Morishita S, Edahiro Y, Takei H, Yoo Y, et al. JAK2, CALR, and MPL mutation spectrum in Japanese patients with myeloproliferative neoplasms. Haematologica. 2015; 100(2): e46-8. https://doi.org/10.3324/haematol.2014.115113 PMid:25398833 PMCid:PMC4803122 DOI: https://doi.org/10.3324/haematol.2014.115113
Murugesan G, Guenther-Johnson J, Mularo F, Cook JR, Daly TM. Validation of a molecular diagnostic assay for CALR exon 9 indels in myeloproliferative neoplasms: Identification of coexisting JAK2 and CALR mutations and a novel 9 bp deletion in CALR. International Journal of Laboratory Hematology. 2016;38(3):284-97. https://doi.org/10.1111/ijlh.12484 PMid:27018326 DOI: https://doi.org/10.1111/ijlh.12484
Broséus J, Lippert E, Harutyunyan AS, Jeromin S, Zipperer E, Florensa L, et al. Low rate of calreticulin mutations in refractory anaemia with ring sideroblasts and marked thrombocytosis. Leukemia. 2014;28(6):1374-6. https://doi.org/10.1038/leu.2014.49 PMid:24476766 DOI: https://doi.org/10.1038/leu.2014.49
Cazzola M, Kralovics R. From Janus kinase 2 to calreticulin: The clinically relevant genomic landscape of myeloproliferative neoplasms. Blood. 2014;123(24):3714-9. https://doi.org/10.1182/blood-2014-03-530865 PMid:24786775 DOI: https://doi.org/10.1182/blood-2014-03-530865
Kang MG, Choi HW, Lee JH, Choi YJ, Choi HJ, Shin JH, et al. Coexistence of JAK2 and CALR mutations and their clinical implications in patients with essential thrombocythemia. Oncotarget. 2016;7(35):57036-49. https://doi.org/10.18632/oncotarget.10958 PMid:27486987 PMCid:PMC5302971 DOI: https://doi.org/10.18632/oncotarget.10958
Barbui T, Finazzi G, Carobbio A, Thiele J, Passamonti F, Rumi E, et al. Development and validation of an International Prognostic Score of thrombosis in World Health Organization-essential thrombocythemia (IPSETthrombosis). Blood. 2012;120(26):5128-33. https://doi.org/10.1182/blood-2012-07-444067 PMid:23033268 DOI: https://doi.org/10.1182/blood-2012-07-444067
Barbui T, Thiele J, Passamonti F, Rumi E, Boveri E, Ruggeri M, et al. Survival and disease progression in essential thrombocythemia are significantly influenced by accurate morphologic diagnosis: A international study. Journal of Clinical Oncology. 2011;29(23):3179-84. https://doi.org/10.1200/JCO.2010.34.5298 PMid:21747083 DOI: https://doi.org/10.1200/JCO.2010.34.5298
Tefferi A, Vainchenker W. Myeloproliferative neoplasms: Molecular pathophysiology, essential clinical understanding, and treatment strategies. Journal of Clinical Oncology. 2011;29(5):573-82. https://doi.org/10.1200/JCO.2010.29.8711 PMid:21220604 DOI: https://doi.org/10.1200/JCO.2010.29.8711
Thiele J, Kvasnicka HM, Müllauer L, Buxhofer-Ausch V, Gisslinger B, Gisslinger H. Essential thrombocythemia versus early primary myelofibrosis: A multicenter study to validate the WHO classification. Blood. 2011;117(21):5710-8. https://doi.org/10.1182/blood-2010-07-293761 PMid:21447832 DOI: https://doi.org/10.1182/blood-2010-07-293761
Downloads

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
The copy rights of the articles published in Colombia Médica belong to the Universidad del Valle. The contents of the articles that appear in the Journal are exclusively the responsibility of the authors and do not necessarily reflect the opinions of the Editorial Committee of the Journal. It is allowed to reproduce the material published in Colombia Médica without prior authorization for non-commercial use

 https://orcid.org/0009-0000-4510-2826
https://orcid.org/0009-0000-4510-2826